 Hepatitis C, Autoimmunity and Gluten
Hepatitis C, Autoimmunity and Gluten
by Jeffrey Dach MD
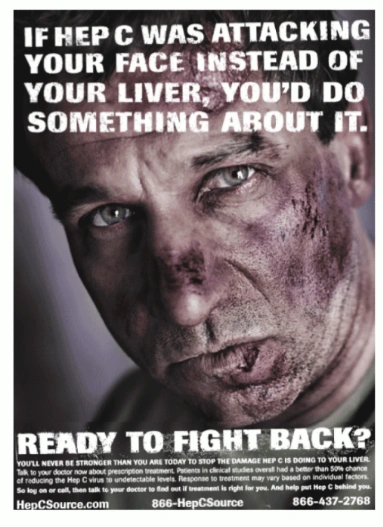
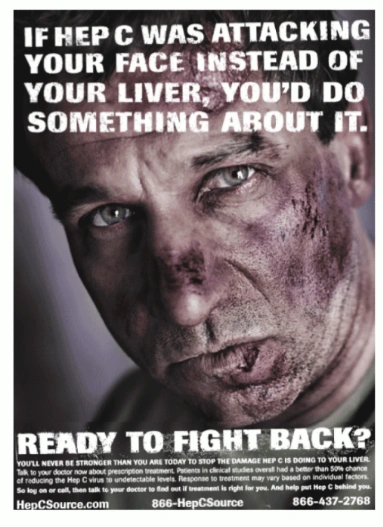
Unethical Advertising for a Disease
Advertisement to draw attention to a disease should raise a red warning flag. A basic rule is that real diseases don’t need any advertising, Only phony or fake diseases require advertising, to increase sales and profits for the drug for the new disease. In my opinion, such advertising is unethical, and these Hepatitis C ads (upper left) have raised ethical concerns. (14-16) Upper Left ad courtesy of Roche.
Case Report:
Jill is a 52 year old nurse who contracted Hepatitis C after a needle stick at the hospital ten years ago. She has done well with occasional mild liver enzyme elevations and fluctuations in her platelet count which always seem to resolve on their own.
In the past, Jill’s doctors have always offered the usual Hepatitis C treatment with interferon and ribaviron. Because of potential adverse side effects , she has so far declined treatment. Now, Jill’s doctors are recommending two new drugs, boceprevir (Victrelis) and telaprevir (Incivek). Jill is asking for advice. What should she do?
Problems with Viral Causation of Hepatitis C
Critics have pointed out viral liver infections with Hepatitis A and B are real diseases in which the virus can be isolated in culture from infected individuals, and animal disease can be produced by injecting the virus into animals. Thirdly, a vaccine against the virus can be produced in the lab. These criteria are called Koch’s postulates, used for one hundred years to prove microbial causation of disease. None of these Koch’s Postulates are satisfied for Hepatitis C, raising questions about the scientific basis for viral causation.
With hepatitis C, Koch’s Postulates have been thrown out the window, changing the diagnosis to a new technique called RNA sequencing with the PCR test (polymerase chain reaction).(17) Modern microbiology has accepted this change, no longer requiring satisfaction of Koch’s Postulates. I would question the validity of this, and instead examine the profit motives involved. Huge amounts of money are at stake in the sale of drugs to treat the new disease.
Asymptomatic Hep C – Outcomes are Mild
Left Image Hep C Ad courtesy of Jon Cox
In a 25-year study of the outcomes of hepatitis C virus infection in 738 people, outcomes were relatively mild: After 25 years, most (85%) had no or mild fibrosis, and only 2% had cirrhosis. Nearly one-fifth spontaneously recovered.(2) These mild outcomes would raise questions about the merits of treating asymptomatic individuals with toxic Hep C treatments.(8)
Is Hepatitis C an Auto-Immune Disease?
Many clinical features of Hepatitis C resemble an auto-immune disease, such as the long duration, chronic nature and association with other auto-immune symptoms.
According to Dr Strassburg, “Based on biochemical and clinical features, Hep C is almost indistinguishable from autoimmune hepatitis,”(4)
Viral causation of Hepatitis C is accepted as dogma by modern
medicine. Will this be modified or overturned in the future and changed
to an autoimmune disease? We will have to wait and see.
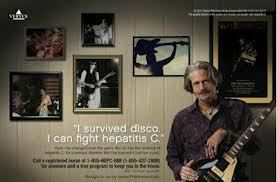 Left Image: Hep C ad posted on the side of a bus features an aging rocker. Courtesy of Vertex Pharmaceuticals Inc.
Left Image: Hep C ad posted on the side of a bus features an aging rocker. Courtesy of Vertex Pharmaceuticals Inc.
Hep C and the Auto-immune and Gluten Connection
In addition to itself being an auto-immune liver disease similar to auto-immune hepatitis, Hepatitis C is associated with various other auto-immune symptoms such as arthralgias, arthritis, vasculitis and sicca syndrome (Sjogrens). (3,4) This type of association might raise the suspicion that Hep C is an auto-immune disease related to gluten exposure and underlying gluten sensitivity. Both gluten sensitivity and celiac disease are known to be associated with autoimmune disease and liver disease.(5,6,7)
According to Kenneth D Fine MD, “hepatitis C appears to be the most common hepatic disease associated with the development of celiac sprue.”(5)
True enough, when one examines the medical literature, Hep C does have a strong association with gluten sensitivity and celiac disease. Surprisingly, conventional drug treatment with interferon may exacerbate the autoimmune features, and activate a previously “Silent Celiac Disease”(6)
What Causes Progression of Hep C ?
Although most Hep C patients have a mild outcome, some will progress to advanced liver disease with 30,000 deaths from cirrhosis and liver failure attributed to Hepatitis C annually. What factors predict progression of disease? We don’t know. However, one such factor has been defined as LPS and Leaky Gut. Hepatitis C has been linked to Leaky Gut, LPS translocation, Gluten sensitivity, and Celiac Disease.(9)
According to Dr Sandler, “LPS-induced local and systemic inflammation is associated with cirrhosis and predicts progression to end-stage liver disease in patients with HBV or HCV infection.”(9)
LPS is lipo-poly-sachharide coating from gram negative bacteria that enter the liver through the portal circulation. They enter because of “leaky gut”. Allesio Fasano’s group at the University of Maryland has worked out the mechanism involved in increased gut permeability (leaky gut), The most common cause for a dysfunctional mucosal barrier (leaky gut) is gluten consumption in genetically predisposed individuals.(18)
If all the above is true, one might argue that all Hep C patients should be tested for LPS antibodies (Cyrex array 2), as well as gluten sensitivity with anti-gliadin antibodies (Cyrex or Enterolabs). One might then expect Hep C liver patients to benefit from a strict gluten free diet as in this report of 4 patients with liver failure who recovered on a gluten free diet.(21)
Hep C and Treatment with LDN
Low Dose Naltrexone (LDN) is beneficial for various autoimmune diseases. therefore benefit in Hepatitis C patients might be expected. (Nola Hepper patient case report )
Burt Berkson MD and Triple Antioxidant Therapy
Burt Berkson MD has shared his experience treating Hep C patients with triple anti-oxidant therapy: alpha lipoic acid, selenium and silymarin with excellent recovery in three patients with advanced liver disease .(19,20)
Hebrew University in Jerusalem – Natural Medicine for Hep C
Dr Melhem from the Liver Unit of Hebrew University reported on natural treatment of Hep C in the 2005 issue of Gasteroenterology.(22) Dr. Melman treated 50 chronic Hep C patients with oral and IV antioxidants over 20 weeks with glycyrrhizin, schisandra, silymarin, ascorbic acid, lipoic acid, L-glutathione, and alpha-tocopherol. Four different intravenous preparations, glycyrrhizin, ascorbic acid, L-glutathione, B-complex were given twice weekly for the first 10 weeks, and followed up for an additional 20 weeks. Normalization of liver enzymes occurred in 44% of patients who had elevated pretreatment ALT levels.(22)
Hepatitis C may Benefit from Phlebotomy
Iron accumulation in liver in patients genetic hemochromatosis can cause mild elevations in liver enzymes on lab testing, and lead to more severe hepatic dysfunction and cirrhosis. Could reduction in iron stores be beneficial for Hepatitis C patients? A study from Japan shows that liver enzymes may normalize in Hepatitis C patients after repeated phlebotomies.(23) Others have confirmed that iron depletion may be beneficial,
Conclusion:
Hep C advertising campaigns raise warning flags and serious ethical concerns about the motivations of the drug companies. Lack of virus isolation from infected individuals and animal models, lack of a vaccine, and failure to satisfy Koch’s Postulates of causation, raise questions about proof of viral causation. The mild clinical outcomes, and long term, chronic auto-immune nature of the illness suggests causation may be auto-immune, or perhaps another cause which is more complex than a simple viral model.
The mild outcomes in asymptomatic individuals with positive Hep C RNA testing raises a question about the merits of treating asymptomatic individuals with expensive drug regimens which carry adverse side effects,
If Hepatitis C causation is autoimmune, then leaky gut, LPS translocation to the liver through the portal circulation, and underlying gluten sensitivity should all be explored with lab testing. This would include gliadin sub fraction antibody testing, and a strict gluten free diet.
There has been renewed interest in natural treatments for Hepatitis C with oral and IV antioxidants, alpha lipoic acid and Low Dose Naltrexone which may improve clinical status without adverse effects.
Update July 2014 – Sovaldi and Gilead
Gilead Sciences Inc. claims its new drug Sovaldi treats Hepatitis C with a cure rate of 90% and with fewer side effects. The drug's hefty price tag may be a deterrent. At $1000 per pill, this makes a 12 week course of treatment a cool $84,000.
Jeffrey Dach MD
Articles with related interest:
Four part series on Gluten and Leaky Gut :
part one
part two
part three
part four
Links and references
1) http://hopefulgeranium.blogspot.com/2011/12/hepatitis-c-gluten-and-folly-of.html
Hepatitis C, Gluten, Casein and the Folly of Agriculture
Gluten and Casein as Factors responsible for the Characteristic Diseases of Chronic Hepatitis C
2) http://www.ncbi.nlm.nih.gov/pubmed/22740714
J Infect Dis. 2012 Sep 1;206(5):654-61.
A 25-year study of the clinical and histologic outcomes of hepatitis C
virus infection and its modes of transmission in a cohort of initially
asymptomatic blood donors.Allison RD, Conry-Cantilena C, Koziol D,
Schechterly C, Ness P, Gibble J, Kleiner DE, Ghany MG, Alter HJ.Source
Department of Transfusion Medicine, National Institutes of Health,
Bethesda, MD, USA.
A total of 738 volunteer blood donors who were positive for
anti-hepatitis C virus (HCV) were assessed for risk factors and outcomes
for up to 15 years within the study and up to 54 years from the
estimated onset of infection.
METHODS:A third-generation recombinant immunoblot assay (RIBA) was
performed to distinguish true from false anti-HCV reactivity. Findings
of HCV polymerase chain reaction classified subjects as having chronic
HCV infection or as having recovered. Liver biopsy specimens were staged
by Ishak fibrosis score and graded by histologic activity index.
RESULTS:Of 738 anti-HCV-positive subjects, 469 (64%) had positive RIBA
results, 217 (29%) had negative results, and 52 (7%) had indeterminate
results. Primary independent risk factors were injection drug use (odds
ratio [OR], 35.0; P < .0001), blood transfusion (OR, 9.9; P <
.0001), and intranasal cocaine use, including 79 “snorters” who
repeatedly denied injection drug use or blood transfusion (OR, 8.5; P
< .0001). Classification and regression tree and random forest
analyses confirmed these risk factors. A total of 384 RIBA-positive
donors (82%) were HCV RNA positive; of these, liver biopsy specimens
from 185 (48%) showed no fibrosis in 33%, mild fibrosis in 52%, bridging
fibrosis in 12%, and cirrhosis in 2% a mean duration of 25 years after
infection. Analysis of 63 repeat biopsy specimens showed that 8%
progressed ≥2 Ishak stages over 5 years (mean progression, 0.06 Ishak
stages/year).
CONCLUSIONS:Injection drug use and blood transfusion
before 1990 are dominant risk factors for HCV acquisition; intranasal
cocaine use may be a surreptitious route of parenteral spread. After a
mean of 25 years of HCV infection, histologic outcomes were relatively mild: 85% had no or mild fibrosis, and only 2% had cirrhosis. Nearly one-fifth spontaneously recovered.
3) http://www.ncbi.nlm.nih.gov/pubmed/22155016
Autoimmun Rev. 2012 Jul;11(9):659-63.
Autoantibodies in patients with chronic hepatitis C virus infection: pitfalls for the diagnosis of rheumatic diseases.
Palazzi C, Buskila D, D’Angelo S, D’Amico E, Olivieri I.
Rheumatology Department of Lucania, San Carlo Hospital of Potenza and Madonna delle Grazie Hospital of Matera, Italy.
Abstract Hepatitis C virus infection (HCV) is one of the best mimes in medicine. About 40-70% of patients suffering from this disorder develop at least one extra-hepatic disorder that can have a rheumatic nature (arthralgias, arthritis, vasculitis and sicca syndrome) and must be differentiated from the primitive rheumatic diseases. In addition, HCV infection can also alter the laboratory tests. Several alterations of first line laboratory tests can be usually found in both chronic HCV infection and chronic inflammatory rheumatic disorders. In the present review we analyze the interference of HCV in tests more specifically used in rheumatology: rheumatoid factor and other autoantibodies (ANA, anti-ENA, ANCA, anti-DNA, antiphospholipid, anti-CCP). In patients suffering from HCV infection, the diagnosis of connective tissue diseases (CTD) or rheumatoid arthritis (RA) should be made only when the detected symptoms or laboratory data are not inducible by HCV, otherwise only a diagnosis of “possible CTD” or “possible RA” should be considered.
4) http://www.ncbi.nlm.nih.gov/pubmed/14550873
Autoimmun Rev. 2003 Oct;2(6):322-31.
Autoimmunity and hepatitis C.
Strassburg CP, Vogel A, Manns MP.
Source Department of Gastroenterology, Hepatology and Endocrinology,
Hannover Medical School, Carl-Neuberg-Str. 1, D-30625 Hannover, Germany.
Abstract Hepatitis C is a widespread chronic liver disease leading to cirrhosis and to the complications of portal hypertension. Based on biochemical and clinical features, it is almost indistinguishable from autoimmune hepatitis, which is characterized by the absence of viral infection, and other causes of chronic liver diseases, and represents a classical autoimmune disease with loss of immunological tolerance of liver tissue. Although the differentiation between both diseases is not difficult due the availability of diagnostic viral markers, it is well recognized that not only are autoantibodies present in autoimmune hepatitis frequently detected in hepatitis C, but also that an array of immune-mediated symptoms and diseases occur in patients with chronic hepatitis C. This has prompted research aimed at identifying a link between hepatitis C and autoimmunity, and autoimmune hepatitis in particular. This review focuses on the general immunological mechanisms linking viral infections with autoimmunity and includes the specific features of hepatitis C- and D-associated autoimmunity. Virus infection remains at the center of molecular and cellular research aimed at identifying the forces driving human autoimmunity and autoimmune diseases.
5) http://www.nature.com/ajg/journal/v96/n1/abs/ajg200124a.html
The American Journal of Gastroenterology (2001) 96, 138–145;
Celiac sprue: another autoimmune syndrome associated with hepatitis C. Kenneth D Fine MD, Frederick Ogunji PhD, Yasser Saloum MD, Shari Beharry BS, Jeffrey Crippin MD and Jeffrey Weinstein MD
Celiac sprue is being diagnosed with increasing frequency by
screening individuals with epidemiologically associated autoimmune
syndromes. We sought to test our hypothesis that hepatitis C also may
predispose to celiac sprue because it can trigger autoimmune reactions.
METHODS:Two hundred fifty-nine consecutively evaluated patients with
chronic hepatitis C infection, 59 with autoimmune liver disease, 137
with other hepatic diseases, 356 with various GI syndromes, and 221
normal volunteers underwent serologic screening for celiac sprue.
Patients with antigliadin, antiendomysial, and antitissue
transglutaminase antibodies in serum underwent duodenoscopy and biopsy.
RESULTS:There was a statistically significantly higher prevalence of
antigliadin antibody in all groups of patients with liver disease
compared with GI controls and normal controls. However, only patients
with hepatitis C (n = 3; 1.2%) or autoimmune liver disease (n = 2; 3.4%)
had antiendomysial/antitissue transglutaminase antibody in serum. One
of 221 normal volunteers (0.4%) was antigliadin, antiendomysial, and
antitissue transglutaminase positive; this individual also was found to
have hepatitis C (previously undiagnosed). Each of these six individuals
had mild intestinal symptoms, duodenal histopathology consistent with
celiac sprue, and the celiac-associated HLA-DQ2 allele. Five of the six
followed a prescribed gluten-free diet and experienced symptomatic
improvement.
CONCLUSION:Celiac sprue is epidemiologically associated with chronic
hepatitis C infection and with autoimmune liver disease. Because
hepatitis C is much more frequently encountered than autoimmune liver
disease, hepatitis C appears to be the most common hepatic disease associated with the development of celiac sprue.
6) http://www.ncbi.nlm.nih.gov/pubmed/15492610
J Clin Gastroenterol. 2004 Nov-Dec;38(10):901-5.
Silent celiac disease in chronic hepatitis C: impact of interferon treatment on the disease onset and clinical outcome.
Durante-Mangoni E, Iardino P, Resse M, Cesaro G, Sica A, Farzati B, Ruggiero G, Adinolfi LE.
Divisions of Internal Medicine and Hepatology, Second University of Naples Medical School, Napoli, Italy.
To assess the impact of interferon treatment on celiac disease onset
in hepatitis C patients and to clarify its clinical relevance and
outcome.
BACKGROUND:Hepatitis C is associated with autoimmunity, which can be exacerbated by interferon treatment. Cases of celiac disease activation during interferon treatment have been reported.
STUDY:Retrospective evaluation of 534 hepatitis C patients with or
without symptoms compatible with celiac disease onset during interferon
treatment and 225 controls. Anti-transglutaminase antibodies were
assayed. HLA-DQA1 and -B1 loci were typed. Upper gastrointestinal
endoscopy was applied to confirm the diagnosis in antibody-positive
patients.
RESULTS:Anti-transglutaminase antibodies were detected before treatment in 1.3% of hepatitis C patients and in 0.4% of controls (not significant). Eighty-six percent of patients with anti-transglutaminase antibodies showed activation of celiac disease while on interferon.
Symptoms ranged from mild to severe, and interferon had to be
discontinued in 2 of 7 (29%) patients. Symptoms disappeared in 6 of 7
patients after interferon withdrawal. Onset of symptoms compatible with
celiac disease during interferon therapy was significantly associated
with the presence of anti-transglutaminase antibodies (OR 53).
CONCLUSIONS:
In hepatitis C patients, the activation of silent celiac disease
during interferon treatment is almost universal and should be
suspected, but it uncommonly requires interferon treatment
discontinuation. Symptoms subside after interferon withdrawal.
7) http://www.ncbi.nlm.nih.gov/pubmed/18231858
Dig Dis Sci. 2008 Aug;53(8):2151-5. doi: 10.1007/s10620-007-0146-1. Epub 2008 Jan 31.
Celiac disease and non-organ-specific autoantibodies in patients with chronic hepatitis C virus infection.
Ruggeri C, La Masa AT, Rudi S, Squadrito G, Di Pasquale G, Maimone S,
Caccamo G, Pellegrino S, Raimondo G, Magazzù G. Cystic Fibrosis and
Paediatric Gastroenterology Unit, Dipartimento di Scienze Pediatriche
Mediche e Chirurgiche, Università di Messina, Messina, Italy.
Considering that celiac disease (CD) is an autoimmune-based entity
and the hepatitis C virus is suspected of being able to trigging
autoimmune reactions, it has been hypothesized that hepatitis C virus
infection might predispose to CD. The aim of this study was to
investigate CD-related antibodies in a large series of hepatitis C
virus-infected subjects that were also tested for non-organ-specific
autoantibodies (NOSA) as indirect marker of autoimmune disorders.
METHODS: Two hundred and forty-four patients with chronic hepatitis C
virus infection (HCV-patients) and 121 patients with HCV-negative liver
disease (non-HCV-patients) underwent NOSA determination and celiac
serology (firstly, anti-tissue transglutaminase antibodies, then the
cases which tested positive were subsequently evaluated for the presence
of antiendomysial antibodies). Serum samples from 42 of the
HCV-patients who underwent interferon-alpha therapy after enrollment
were tested for celiac antibodies and NOSA even after stopping
treatment. Additionally, sera from 1,230 blood donors were assayed for
celiac serology as healthy control population.
RESULTS: Positive anti-endomysial antibodies (AEA) were found in 5/244 (2%) HCV-patients, 1/121 (0.8%) non-HCV-patients and 2/1,230 (0.16%) blood donors, with a significant difference between HCV-patients and blood donors (P = 0.02; Odds ratio 12.8;
95% Confidence Interval 2.4-66). NOSA were found in 51 HCV-patients but
only one of them had positive AEA. Eight out of 42 HCV-patients treated
with interferon-alpha developed NOSA under therapy and none of them had
CD antibodies.
CONCLUSIONS:
AEA occur in 2% of HCV-patients and their presence is independent of other patterns of autoimmunity.
————————————————–
8) http://www.sciencemag.org/content/285/5424/26.summary
The Scientific Challenge of Hepatitis C Jon Cohen Science 1999 285: 26-30. (in News Focus
for HCV there appears to be no such thing as a typical infection. The
severity of the disease varies greatly from person to person and–to the
frustration of clinicians and patients–there are few reliable indicators
to predict who will do well or badly.
Evidence accumulated over the past few years indicates that the immune
systems of 15% to 25% of people infected with HCV will overcome the
virus during the initial infection and clear it from the bloodstream.
The remaining 75% to 85% will develop a chronic infection.
NIH’s Alter and Jay Hoofnagle from the National Institute of Diabetes
and Digestive and Kidney Diseases (NIDDK) reported results from a 7-year
study of more than 400 would-be blood donors who had tested positive
for HCV and whose infection could, in most cases, be traced to a
transfusion or injection. Even though they had been infected for an average of nearly 20 years, only 13% had severe fibrosis and a mere 2% had cirrhosis.
These results closely match those from an Irish study published in the
22 April New England Journal of Medicine that charted disease
progression over 17 years in 376 women who had received contaminated
blood products in the 1970s. And a study by NIDDK’s Leonard Seeff looked
at 8568 blood samples stored by the U.S. Air Force between 1948 and
1954 and found that 17 tested positive for HCV antibodies; current
records revealed that only one of those infected individuals (5.8%) died
from liver disease.
LPS Leaky Gut – makes Hep C prognosis Worse
Gluten Connection ?
9) http://www.ncbi.nlm.nih.gov/pubmed/21726511
Gastroenterology. 2011 Oct;141(4):1220-30, 1230.e1-3.
Host response to translocated microbial products predicts outcomes of patients with HBV or HCV infection.
Sandler NG, Koh C, Roque A, Eccleston JL, Siegel RB, Demino M, Kleiner DE, Deeks SG, Liang TJ, Heller T, Douek DC.
Source Human Immunology Section, Vaccine Research Center, National
Institute of Allergy and Infectious Diseases, National Institutes of
Health, Bethesda, Maryland 20892, USA.
Chronic infection with hepatitis B or C virus (HBV or HCV) is a leading cause of cirrhosis by unknown mechanisms of pathogenesis.
Translocation of gut microbial products into the systemic circulation
might increase because of increased intestinal permeability, bacterial
overgrowth, or impaired clearance of microbial products by Kupffer
cells. We investigated whether the extent and progression of liver
disease in patients with chronic HBV or HCV infection are associated
with microbial translocation and subsequent activation of monocytes.
METHODS:in a retrospective study, we analyzed data from 16 patients with
minimal fibrosis, 68 with cirrhosis, and 67 uninfected volunteers. We
analyzed plasma levels of soluble CD14 (sCD14), intestinal fatty acid
binding protein, and interleukin-6 by enzyme-linked immunosorbent assay,
and lipopolysaccharide (LPS) by the limulus amebocyte lysate assay, at presentation and after antiviral treatment.
RESULTS:Compared with uninfected individuals, HCV- and HBV-infected individuals had higher plasma levels of LPS,
intestinal fatty acid binding protein (indicating enterocyte death),
sCD14 (produced upon LPS activation of monocytes), and interleukin-6. Portal hypertension, indicated by low platelet counts, was associated with enterocyte death
(P=.045 at presentation, P<.0001 after therapy). Levels of sCD14
correlated with markers of hepatic inflammation (P=.02 for aspartate
aminotransferase, P=.002 for ferritin) and fibrosis (P<.0001 for
γ-glutamyl transpeptidase, P=.01 for alkaline phosphatase, P<.0001
for α-fetoprotein). Compared to subjects with minimal fibrosis, subjects
with severe fibrosis at presentation had higher plasma levels of sCD14
(P=.01) and more hepatic CD14+ cells (P=.0002); each increased risk for
disease progression (P=.0009 and P=.005, respectively).
CONCLUSIONS:LPS-induced local and systemic inflammation is
associated with cirrhosis and predicts progression to end-stage liver
disease in patients with HBV or HCV infection.
10) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC415836/
J Virol. 2004 June; 78(11): 5867–5874.
Hepatitis C Virus Persistence after Spontaneous or Treatment-Induced Resolution of Hepatitis C
Tram N. Q. Pham,1 Sonya A. MacParland,1 Patricia M. Mulrooney,1 Helen
Cooksley,2 Nikolai V. Naoumov,2 and Tomasz I. Michalak1,3,*Molecular
Virology and Hepatology Research, Division of Basic Medical Science,
11) https://sites.google.com/site/jccglutenfree/liverdisease2
Liver and Pancreas Disease The Gluten File
LDN for Hep C – autoimmune disorder
12) http://nolahepper.blogspot.com/2010/06/treating-hepatitis-c-with-low-dose.html
NOLA Hepper - Living in New Orleans, Louisiana with Hepatitis C and
how taking Low Dose Naltrexone (LDN)to treat it is giving me back my
life.
13) http://www.myspace.com/georgedhenderson/blog/536199261
Hepatitis C, Gluten, Casein and the Folly of Agriculture Ron Hoggan, 1997
Gluten and Casein as Factors responsible for the Characteristic Diseases of Chronic Hepatitis C
It so happens that the auto-immune symptoms associated with celiac and
gluten sensitivity diseases, including liver and gall-bladder disease,
and which usually resolve slowly on a strict gluten and dairy-free diet,
are essentially identical to the various syndromes seen in chronic Hep C, especially during or after interferon-alpha treatment.
————————————–
Unethical Advertising
14) http://abcnews.go.com/Health/story?id=117868&page=1#.UXHHzzdaZac
FDA to Examine Hepatitis C Campaign
W A S H I N G T O N, Sept. 14
(ad image of bruised face)
15) http://amarillo.com/stories/111200/tex_healthoff.shtml
Roche Launches New Campaign to Educate Consumers About Hepatitis C
NUTLEY, New Jersey (July 26, 2005) – Roche announced today the launch of
a major new campaign to motivate hepatitis C patients who have been
diagnosed with the disease to take the critical step of discussing
prescription treatment with a liver specialist or hepatitis C-treating
physician.
16) http://www.natap.org/2005/HCV/072905_01.htm
Health officials demand changes in hepatitis C ads
Posted: Sunday, November 12, 2000
17) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC172879/
Clin Microbiol Rev. 1996 January; 9(1): 18–33.
Sequence-based identification of microbial pathogens: a reconsideration
of Koch’s postulates.D N Fredericks and D A Relman Department of
Medicine, Stanford University School of Medicine, California 94305,
USA. Over 100 years ago, Robert Koch introduced his ideas about how to
prove a causal relationship between a microorganism and a disease.
Koch’s postulates created a scientific standard for causal evidence that
established the credibility of microbes as pathogens and led to the
development of modern microbiology. In more recent times, Koch’s
postulates have evolved to accommodate a broader understanding of the
host-parasite relationship as well as experimental advances. Techniques
such as in situ hybridization, PCR, and representational difference
analysis reveal previously uncharacterized, fastidious or uncultivated,
microbial pathogens that resist the application of Koch’s original
postulates, but they also provide new approaches for proving disease
causation. In particular, the increasing reliance on sequence-based methods for microbial identification requires a reassessment of the original postulates and
the rationale that guided Koch and later revisionists. Recent
investigations of Whipple’s disease, human ehrlichiosis, hepatitis C,
hantavirus pulmonary syndrome, and Kaposi’s sarcoma illustrate some of
these issues. A set of molecular guidelines for establishing disease
causation with sequence-based technology is proposed, and the importance
of the scientific concordance of evidence in supporting causal
associations is emphasized.
18) http://www.ncbi.nlm.nih.gov/pubmed/22731712
Ann N Y Acad Sci. 2012 Jul;1258:25-33.
Zonulin, regulation of tight junctions, and autoimmune diseases. Fasano
A. Mucosal Biology Research Center and Center for Celiac Research,
University of Maryland School of Medicine, Baltimore, Maryland, USA.
19) http://www.townsendletter.com/Dec2007/alphalipo1207.htm
Alpha Lipoic Acid and Liver Disease
by Burton M. Berkson, MD, MS, PhD
20) http://www.ncbi.nlm.nih.gov/pubmed/10554539
Med Klin (Munich). 1999 Oct 15;94 Suppl 3:84-9.
A conservative triple antioxidant approach to the treatment of hepatitis
C. Combination of alpha lipoic acid (thioctic acid), silymarin, and
selenium: three case histories. Berkson BM. Integrative Medical Center
of New Mexico, New Mexico State University, Las Cruces, USA.
There has been an increase in the number of adults seeking liver transplantation for hepatitis C in the last few years and the count is going up rapidly. There is no reliable and effective therapy for chronic hepatitis C since interferon and antivirals work no more than 30% of the time, and liver transplant surgery is uncertain and tentative over the long run. This is because, ultimately, residual hepatitis C viremia infects the new liver. Furthermore, liver transplantation can be painful, disabling and extremely costly. TREATMENT PROGRAM:
The author describes a low cost and efficacious treatment program in 3 patients with cirrhosis, portal hypertension and esophageal varices secondary to chronic hepatitis C infection.
This effective and conservative regimen combines 3 potent antioxidants
(alpha-lipoic acid [thioctic acid], silymarin, and selenium) that
possess antiviral, free radical quenching and immune boosting qualities.
CONCLUSION: There are no remarkably effective treatments for chronic hepatitis C in general use. Interferon and antivirals have less than a 30% response rate
and because of the residual viremia, a newly transplanted liver usually
becomes infected again. The triple antioxidant combination of
alpha-lipoic acid, silymarin and selenium was chosen for a conservative
treatment of hepatitis C because these substances protect the liver from
free radical damage, increase the levels of other fundamental
antioxidants, and interfere with viral proliferation. The 3
patients presented in this paper followed the triple antioxidant program
and recovered quickly and their laboratory values remarkably improved.
Furthermore, liver transplantation was avoided and the patients are
back at work, carrying out their normal activities, and feeling healthy.
The author offers a more conservative approach to the treatment of
hepatitis C, that is exceedingly less expensive. One year of the triple
antioxidant therapy described in this paper costs less than $2,000, as
compared to mor than $300,000 a year for liver transplant surgery. It
appears reasonable, that prior to liver transplant surgery evaluation,
or during the transplant evaluation process, the conservative triple
antioxidant treatment approach should be considered. If these is a
significant betterment in the patient’s condition, liver transplant
surgery may be avoided.
21) http://www.ncbi.nlm.nih.gov/pubmed/11910339
Gastroenterology. 2002 Apr;122(4):881-8.
Celiac disease in patients with severe liver disease: gluten-free diet
may reverse hepatic failure. Kaukinen K, Halme L, Collin P, Färkkilä M,
Mäki M, Vehmanen P, Partanen J, Höckerstedt K. Department of Internal
Medicine, Tampere University Hospital, Tampere, Finland.
Mild liver abnormalities are common in patients with celiac disease
and usually resolve with a gluten-free diet. We investigated the
occurrence of celiac disease in patients with severe liver failure.
METHODS: Four patients with untreated celiac disease and severe liver
disease are described. Further, the occurrence of celiac disease was
studied in 185 adults with previous liver transplantation using serum
immunoglobulin A endomysial and tissue transglutaminase antibodies in
screening.
RESULTS: Of the 4 patients with severe liver disease and celiac
disease, 1 had congenital liver fibrosis, 1 had massive hepatic
steatosis, and 2 had progressive hepatitis without apparent origin.
Three were even remitted for consideration of liver transplantation.
Hepatic dysfunction reversed in all cases when a gluten-free diet was
adopted. In the transplantation group, 8 patients (4.3%) had celiac
disease. Six cases were detected before the operation: 3 had primary
biliary cirrhosis, 1 had autoimmune hepatitis, 1 had primary sclerosing
cholangitis, and 1 had congenital liver fibrosis. Only 1 patient had
maintained a long-term strict gluten-free diet. Screening found 2 cases
of celiac disease, 1 with autoimmune hepatitis and 1 with secondary
sclerosing cholangitis.
CONCLUSIONS: The possible presence of celiac disease should be
investigated in patients with severe liver disease. Dietary treatment
may prevent progression to hepatic failure, even in cases in which liver
transplantation is considered.
22) http://www.ncbi.nlm.nih.gov/pubmed/16082287
J Clin Gastroenterol. 2005 Sep;39(8):737-42.
Treatment of chronic hepatitis C virus infection via antioxidants:
results of a phase I clinical trial. Melhem A, Stern M, Shibolet O,
Israeli E, Ackerman Z, Pappo O, Hemed N, Rowe M, Ohana H, Zabrecky G,
Cohen R, Ilan Y.
Source Liver Unit, Department of Medicine, Hebrew University, Hadassah Medical Center, Jerusalem, Israel.
The pathogenesis of chronic hepatitis C virus (HCV) infection is
associated with a defective host antiviral immune response and
intrahepatic oxidative stress. Oxidative stress and
lipid peroxidation play major roles in the fatty liver accumulation
(steatosis) that leads to necro-inflammation and necrosis of hepatic
cells. Previous trials suggested that antioxidative therapy may have a
beneficial effect on patients with chronic HCV infection.
To determine the safety and efficacy of treatment of chronic HCV patients via a combination of antioxidants.
Fifty chronic HCV patients were treated orally on a daily basis for 20 weeks with seven
antioxidative oral preparations (glycyrrhizin, schisandra, silymarin,
ascorbic acid, lipoic acid, L-glutathione, and alpha-tocopherol), along
with four different intravenous preparations (glycyrrhizin, ascorbic
acid, L-glutathione, B-complex) twice weekly for the first 10 weeks, and
followed up for an additional 20 weeks. Patients were
monitored for HCV-RNA levels, liver enzymes, and liver histology.
Assessment of quality of life was performed using the SF-36
questionnaire.
RESULTS:In one of the tested parameters (eg, liver enzymes, HCV RNA
levels, or liver biopsy score), a combination of antioxidants induced a
favorable response in 48% of the patients (24). Normalization
of liver enzymes occurred in 44% of patients who had elevated
pretreatment ALT levels (15 of 34). ALT levels remained normal
throughout follow-up period in 72.7% (8 of 11). A decrease
in viral load (one log or more) was observed in 25% of the patients
(12). Histologic improvement (2-point reduction in the HAI score) was
noted in 36.1% of the patients. The SF-36 score improved in 26 of 45
patients throughout the course of the trial (58% of the patients).
Treatment was well tolerated by all patients. No major adverse reactions
were noted.
CONCLUSIONS: These data suggest that multi antioxidative treatment in
chronic HCV patients is well tolerated and may have a beneficial effect
on necro-inflammatory variables. A combination of antiviral and
antioxidative therapies may enhance the overall response rate of these
patients.
23) http://www.ncbi.nlm.nih.gov/pubmed/16211347
J Gastroenterol. 2005 Sep;40(9):901-6.
Determinants of serum ALT normalization after phlebotomy in patients with chronic hepatitis C infection.
Kawamura Y, Akuta N, Sezaki H, Hosaka T, Someya T, Kobayashi M, Suzuki F, Suzuki Y, Saitoh S, Arase Y, Ikeda K, Kumada H.
Source Department of Gastroenterology, Toranomon Hospital, 2-2-2 Toranomon, Minato-ku, Tokyo 105-8470, Japan.
Abstract BACKGROUND:Phlebotomy is performed to reduce excessive iron
accumulation in hepatic tissue. We studied serum alanine
aminotransferase (ALT) normalization rates and 50% reduction in initial
serum ALT (ALT(50%) reduction rate) in patients with hepatitis C viral
(HCV) infection and investigated the factors that influenced the
response to phlebotomy therapy.
METHODS:We evaluated 23 consecutive patients with HCV infection who
underwent phlebotomy. Phlebotomy was performed a few times per week,
then a few times per month, and 200-400 ml of blood was removed at each
session, depending on the clinical response. During the course of
therapy, hemoglobin (Hb), serum ALT, and ferritin levels were assessed
monthly.
RESULTS:In patients with Hb of less than 11 g/dl, the ALT(50%) reduction
rate was 87.5%. In patients with a serum ferritin level of less than 10
g/dl the ALT(50%) reduction rate was 83.3%. In patients with Hb of less
than 11 g/dl, the ALT normalization rate was 50%, and in those with a
serum ferritin level of less than 10 g/dl, the ALT normalization rate
was 41.7%. Multivariate analysis identified ALT less than 100 IU/l at
the start of phlebotomy as an independent factor associated with ALT
normalization. Of the 7 patients who showed no response to phlebotomy,
85.7% were obese (body mass index > or =25 kg/m(2)), and 40% showed
more than 30% steatosis on liver histology. The cumulative ALT
normalization rate in relation to the total volume of blood loss was
43.9% with a blood less or more than 3 l, and thus was optimal above 3
l.
CONCLUSIONS:Although the sample number was relatively small, the results
of our study suggest that phlebotomy is effective therapy for HCV
patients who are nonobese, show little or no steatosis on liver
histology, and have a baseline serum ALT level of less than 100 IU/l.
Jeffrey Dach MD
7450 Griffin Road, Suite 190
Davie, Fl 33314
954-792-4663
www.jeffreydach.com
www.drdach.com
www.naturalmedicine101.com
www.bioidenticalhormones101.com
www.truemedmd.com
www.bioidenticalmds.com
Click Here for: Dr Dach’s Online Store for Pure Encapsulations Supplements
Click Here for: Dr Dach’s Online Store for Nature’s Sunshine Supplements
Web Sites and Discussion Board Links:
jdach1.typepad.com/blog/
disc.yourwebapps.com/Indices/244124.html
disc.yourwebapps.com/Indices/244066.html
disc.yourwebapps.com/Indices/244067.html
disc.yourwebapps.com/Indices/244161.html
disc.yourwebapps.com/Indices/244163.html
disc.yourwebapps.com/Indices/244163.html
health-forums.1
health-forums.2
Disclaimer click here: www.drdach.com/wst_page20.html
The reader is advised to discuss the comments on these pages with his/her personal physicians and to only act upon the advice of his/her personal physician. Also note that concerning an answer which appears as an electronically posted question, I am NOT creating a physician — patient relationship. Although identities will remain confidential as much as possible, as I can not control the media, I can not take responsibility for any breaches of confidentiality that may occur.
Link to this article:http://wp.me/p3gFbV-gd
Copyright (c) 2013 Jeffrey Dach MD All Rights Reserved. This article may be reproduced on the internet without permission, provided there is a link to this page and proper credit is given.
FAIR USE NOTICE: This site contains copyrighted material the use of which has not always been specifically authorized by the copyright owner. We are making such material available in our efforts to advance understanding of issues of significance. We believe this constitutes a ‘fair use’ of any such copyrighted material as provided for in section 107 of the US Copyright Law. In accordance with Title 17 U.S.C. Section 107, the material on this site is distributed without profit to those who have expressed a prior interest in receiving the included information for research and educational purposes.