Chapter 8. Abandoning the Synthetic Hormone Ship
 Chapter
8:
Chapter
8:
Abandoning the
Synthetic Hormone Ship
Shirley is 52, and suffering from menopausal symptoms of hot flashes, night sweats, insomnia and mood disturbance. The first chance she had, Shirley asked her doctor for bioidentical hormones. Instead, her doctor offered a prescription for Lexapro™, an SSRI antidepressant. Shirley declined the prescription and ran out the door crying all the way home. A few days later, Shirley was sitting in my office asking, "Why won't my doctor give me what I want, bioidentical hormones?"
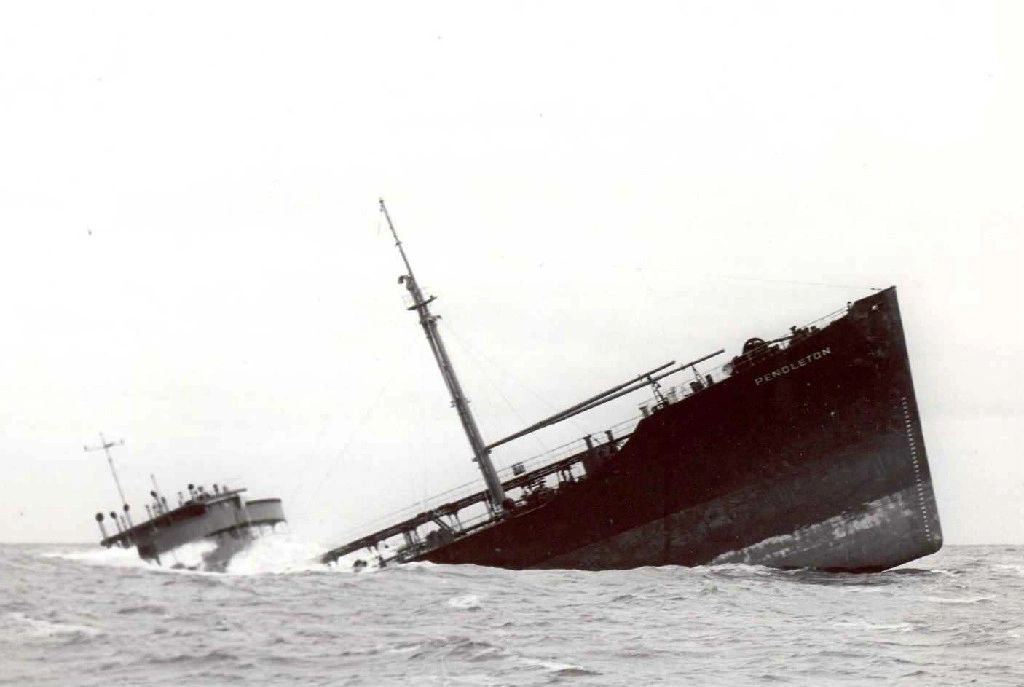
Caption : Abandon Ship, Sinking Ship: Bow section of tanker SS Pendleton grounded near Pollock Rib lightship six miles off Chatham, Mass on the morning of Feb. 19, 1952." Courtesy of Wikimedia Commons.
Ghost Writing – A Shocking Medical Scandal
I explained to Shirley that her doctor’s opinion is shaped by misleading
information in medical journals corrupted by a technique called medical
ghostwriting, a shocking scandal uncovered by Senator Grassley’s
Committee.(1) In this sinister practice, the prestigious name of an
academic MD “opinion leader” appears as author. However, unknown to the
reader, the article is actually written by the drug company’s paid-for-hire
writers. Grassley discovered that sixty articles on women’s hormones were
ghostwritten, downplaying the adverse effects of synthetic hormones, and
casting doubts about bioidentical hormones. Medical ghostwriting is
scientific misconduct and fraud which harms society and corrupts the medical
literature.
A Brief History of Synthetic Hormones – Re-Living the Nightmare
The following is a short history of synthetic hormone replacement as brought to
you by the Drug Industry. (2) Many people have forgotten about the
disaster of DES, Diethylstilbestrol, the first synthetic hormone invented in
1938. This carcinogenic, monster hormone was approved by the FDA and
given to millions of women from 1940 until it was banned in 1975 when it
was shown carcinogenic, causing cervical cancer. The first
reports of cervical cancer in the daughters of DES treated women were published
in April 1971 in the New England Journal of Medicine.(3-4)
Next, the Drug Industry invented Premarin, a horse estrogen isolated from the
urine of pregnant horses. Available since FDA approval in 1942,
Premarin has caused an estimated 15,000 cases of endometrial cancer,
representing the largest epidemic of serious iatrogenic disease ever
reported.(5-8) One might think this would be the end of any
drug. However Premarin was promptly rehabilitated with the addition
of another synthetic hormone, a progestin, to prevent endometrial cancer.
Thus, in 1995, Prempro was born, a synthetic hormone pill containing both
Premarin (the horse estrogen) and Provera (the progestin). Again, this
was FDA approved, thought safe and handed out freely to millions of women.
However, storm clouds soon appeared on the horizon when four large scale
studies showed increased breast cancer and heart disease from this
estrogen-progestin combination pill. The Breast Cancer Detection
Demonstration Project, published in 2000, showed an eight fold increase in
breast cancer for estrogen-progestin users.(9) The Swedish Record Review,
published in 1996, had a fourfold increase in breast cancer with progestin
use.(10) The Million Woman study, published in Lancet in 2003, had a
fourfold increase in breast cancer for estrogen-progestin combination users
compared to estrogen alone users.(11) The brakes came on to this
synthetic hormone experiment in 2002 with the JAMA publication of the Women’s
Health Initiative (WHI), an NIH funded study terminated early because of
increased breast cancer and heart disease in the estrogen-progestin users.(12)
Abandoning the Synthetic Hormone Ship
Two important things happened after this 2002 WHI study was published.
Smart women abandoned synthetic hormones and switched in large number to
bioidentical hormones, producing an immediate decline in breast cancer rates of
about nine per cent.(13,14) A second important thing happened.
Apparently, women have decided to turn to lawyers to protect them, since the
FDA has been unable to do so. Thirteen thousand women have filed cases in
court claiming synthetic hormones caused their breast cancer. These cases
are slowly working their way through the court system, and the jury is still
out, so stay tuned.(15)
Dispelling the Myths and Misconceptions
Over the years, I have compiled a list of myths and misinformation commonly
encountered about bioidentical hormones in newspapers and magazines. Here
are a few of them, followed by the corrections. The misinformation is in
italics, with the correct information to follow.
Myth Number One: "The term bioidentical hormone is undefined and
has no meaning."
This is incorrect. Bioidentical is a term which is defined as having the
exact same chemical structure as hormones found naturally in the human
body. Bioidentical Hormones are the ones circulating in your blood
stream right now.
Myth Number Two: "There is no proof that Bioidentical Hormones
are safer and more effective than synthetic hormones...All of the evidence that
we have suggests that all of these hormones should be painted with the same
brush,”
This is incorrect and misleading. As we have seen in the above short
history of synthetic hormones, there exists a large body of science showing
that synthetic chemically altered hormones cause cancer and heart
disease.(9-14) On the other hand, medical studies have found bioidentical
hormones are safe with no increase in breast cancer or heart disease compared
to non-hormone users. (33-41) An excellent review of this medical science
can be found in a 2009 article by Kent Holtorf MD in Postgraduate Medicine.
(16)
Myth Number Three: "Bioidentical Hormones are not FDA
approved."
This is blatantly incorrect. There are twenty or so FDA approved
bioidentical hormone preparations widely available at corner drug stores. Here
are a few examples: Vivelle-Dot™, Estrace™, Climara™, Prometrium™,
Androgel™ , etc.
Myth Number Four: "Bioidentical Hormones made by compounding
pharmacies are Non-FDA approved."
This is not only incorrect, it is misleading and deceptive. Compounding
pharmacies are regulated at the state level, and do not fall under FDA
jurisdiction. So, of course compounding is not FDA approved.
No FDA approval is required or even desired. Your local hospital pharmacy
is a compounding pharmacy that makes up life saving medication such as IV
antibiotics with no FDA oversight or “approval”. The FDA approval process
is designed for manufactured capsules and tablets, and is impractical and
unnecessary for compounded medications prepared to order by hand.
Are we going to reject IV antibiotics from the hospital pharmacy because these
are non-FDA approved compounded medication? Of course not.
Compounding is here to stay.
Myth Number Five: "Unless a woman has symptoms of hot flashes and
night sweats, she doesn’t need hormones."
This is incorrect. In addition to night sweats and hot flashes, there
are many other valid symptoms of hormone deficiency such as insomnia, cognitive
dysfunction, menopausal arthritis, evaporative dry eye, anxiety, panic, mood
disorder, vaginal dryness, and decreased libido and post hysterectomy.
These are all good indications for prescribing bioidentical hormones. (17-25)
Myth Number Six: "The idea that Menopause is a Hormone
Deficiency Disease was disproven, and the idea that hormone replacement
rejuvenates youth, or prevents degenerative diseases is also
disproven….Hormones decline with age, and is normal and does not require
treatment."
This is incorrect. There is no question that hormonal decline is a health risk.
Three separate studies have shown low testosterone in males carries a 40%
increase in mortality.(26-28) Studies in females show the same findings,
with low hormone levels in women after hysterectomy associated with increased
mortality. (29-30) Hormonal decline is a direct cause of degenerative
diseases of aging, all of which may be prevented or partially reversed by
replenishing hormone levels, a vastly more effective treatment which competes
directly with the Drug Industry.(42-46)
Myth Number Seven: "Hot flashes and sweats in menopausal women
can be treated with SSRI antidepressants. They don’t need to use
hormones."
This is not only wrong, it is criminal. The use of SSRI antidepressants for
menopausal symptoms is NOT FDA approved, and is a cruel mistreatment and
medical victimization of women. This practice should be halted
immediately. Studies of SSRI drugs show they are no better than placebo
for most cases of depression(31), and they are not much better than placebo for
menopausal hot flashes. (32) Synthetic hormones are bad enough, they
cause cancer and heart disease. SSRI drugs like Lexepro™, Effexor™
and Pristiq™ are even worse; they are chemically addictive with horrendous
withdrawal effects. Avoid becoming a medical victim. Stay away.
In Conclusion:
It is time to awaken from the nightmare of synthetic hormones, known for
decades to cause cancer and heart disease. You can put lipstick on a pig,
and it is still a pig. The drug industry can spin, deceive, and
misleading the medical journals and media. Yet, after all the lies and
propaganda, synthetic hormones remain monsters that should be
avoided. Smart women have made the switch to safer and more
effective bioidentical hormones. The future of medicine is your choice to
make. It is recommended you work closely with a knowledgeable physician
before making any decisions regarding hormone treatment. Please feel free
to share this chapter with your doctor.
Articles with Related Interest:
The Safety of Bio-Identical Hormones
The Importance of BioIdentical Hormones
Bioidentical Hormones Prevent Arthritis
Bioidentical Hormone Estrogen Prevents Heart Disease
Morning Rounds With Steven Economou MD
Waking Up from the Synthetic Hormone Nightmare
HRT Does Not Cause Breast Cancer
References for Chapter 8, Abandoning the Synthetic Hormone Ship.(1) http://grassley.senate.gov/about/upload/Senator-Grassley-Report.pdf Ghostwriting in Medical Literature Minority Staff Report 111th Congress United States Senate Committee on Finance Sen. Charles E. Grassley, Ranking Member June 24, 2010
(2) http://www.nytimes.com/2009/12/13/business/13drug.html Menopause, as Brought to You by Big Pharma By NATASHA SINGER and DUFF WILSON Published: December 12, 2009
(3) http://www.nejm.org/doi/pdf/10.1056/NEJM197104222841604 Adenocarcinoma of the Vagina — Association of Maternal Stilbestrol Therapy with Tumor Appearance in Young Women. Arthur L. Herbst, M.D., Howard Ulfelder, M.D., and David C. Poskanzer, M.D. N Engl J Med 1971; 284:878-881April 22, 1971
(4) http://www.jstor.org/pss/2683841 Epidemiologic Evidence for Adverse Effects of DES Exposure during Pregnancy Theodore Colton and E. Robert Greenberg The American Statistician Vol. 36, No. 3, Part 2: Proceedings of the Sixth Symposium on Statistics and the Environment (Aug., 1982), pp. 268-272
(5) http://ajph.aphapublications.org/cgi/reprint/70/3/264.pdf The Epidemic of Endometrial Cancer:A Commentary Hershel Jick et al.Am J Public Health 70:264-267, 1980.
(6) http://www.nejm.org/doi/full/10.1056/NEJM197512042932303 Increased Risk of Endometrial Carcinoma among Users of Conjugated Estrogens. Harry K. Ziel, M.D., and William D. Finkle, Ph.D. N Engl J Med 1975; 293:1167-1170 December 4, 1975
(7) http://www.ncbi.nlm.nih.gov/pubmed/213722 N Engl J Med. 1979 Jan 4;300(1):9-13. Endometrial cancer and estrogen use. Report of a large case-control study. Antunes CM, Strolley PD, Rosenshein NB, Davies JL, Tonascia JA, Brown C, Burnett L, Rutledge A, Pokempner M, Garcia R.
(8) http://www.ncbi.nlm.nih.gov/pubmed/3358913
The dose-effect relationship between 'unopposed' oestrogens and endometrial mitotic rate: its central role in explaining and predicting endometrial cancer risk.Key TJ, Pike MC.
Br J Cancer. 1988 Feb;57(2):205-12.
(9) http://jama.ama-assn.org/content/283/4/485.abstract Menopausal Estrogen and Estrogen-Progestin Replacement Therapy and Breast Cancer Risk. Catherine Schairer, PhD et al. JAMA. 2000;283(4):485-491.
(10) http://onlinelibrary.wiley.com/doi/10.1002/(SICI)1097-0215(19960729)67:3%3C327::AID-IJC4%3E3.0.CO;2-T/pdf
see also http://www.ncbi.nlm.nih.gov/pubmed/8707404
Cancer incidence and mortality in women receiving estrogen and
estrogen-progestin replacement therapy—long-term follow-up of a Swedish
cohort. Ingemar Persson et al. International Journal of Cancer Volume 67,
Issue 3, pages 327–332, 29 July 1996
(11) http://www.ncbi.nlm.nih.gov/pubmed/12927427 Lancet. 2003
Aug 9;362(9382):419-27. Breast cancer and hormone-replacement therapy in the
Million Women Study. Beral V; Million Women Study Collaborators.
(12) http://jama.ama-assn.org/cgi/content/abstract/288/3/321
Risks and Benefits of Estrogen Plus Progestin in Healthy Postmenopausal Women
Principal Results From the Women's Health Initiative Randomized Controlled
Trial
Writing Group for the Women's Health Initiative Investigators JAMA.
2002;288:321-333.
(13) http://www.nejm.org/doi/full/10.1056/NEJMsr070105 The Decrease in Breast-Cancer
Incidence in 2003 in the United States. Peter M. Ravdin, Ph.D., M.D et al. N
Engl J Med 2007; 356:1670-1674 April 19, 2007. A comparison of incidence
rates in 2001 with those in 2004 (omitting the years in which the incidence was
changing) showed that the decrease in annual age-adjusted incidence was 8.6% .
(14) http://jnci.oxfordjournals.org/content/early/2010/09/23/jnci.djq345.abstract Breast Cancer Incidence and
Hormone Replacement Therapy in Canada by Prithwish De, C. Ineke Neutel, Ivo
Olivotto and Howard Morrison. JNCI J Natl Cancer Inst (2010) . This drop
occurred concurrently with a 9.6% decline in the incidence rate of breast
cancer
(15) http://www.bloomberg.com/news/2010-08-27/pfizer-settles-arkansas-prempro-case-before-retrial-over-punitive-damages.html Pfizer Said to Pay $330 Million
to Settle Prempro Lawsuits Claiming Cancer By Jef Feeley - Feb 9, 2011 4:42 PM
ET
(16)http://jeffreydach.com/files/80618-70584/The_Bioidentical_Hormone_Debate_Ken_Holtorf_MD.pdf
Postgraduate Medicine: Volume 121: No.1 January 2009. The Bioidentical Hormone
Debate:Are Bioidentical Hormones (Estradiol, Estriol, and Progesterone) Safer
or More Efficacious than Commonly Used Synthetic Versions in Hormone
Replacement Therapy? Kent Holtorf, MD
(17) http://www.ncbi.nlm.nih.gov/pubmed/11386980 Arch Gen Psychiatry. 2001
Jun;58(6):529-34. Efficacy of estradiol for the treatment of depressive
disorders in perimenopausal women: a double-blind, randomized,
placebo-controlled trial. by Soares CN et al.
(18) http://www.neurology.org/cgi/content/abstract/57/4/605 Neurology 2001;57:605-612, 2001
American Academy of Neurology High-dose estradiol improves cognition for
women with AD Results of a randomized study by S. Asthana, MD et al.
(19) http://www.ncbi.nlm.nih.gov/pubmed/19804793 Estradiol reduces anxiety- and
depression-like behavior of aged female mice by Alicia A. Walf and Cheryl A.
Frye Neuroscience
(20) http://www.ncbi.nlm.nih.gov/pubmed/16142740 Arthritis Rheum.
2005 Sep;52(9):2594-8. Aromatase inhibitors and the syndrome of arthralgias
with estrogen deprivation. Felson DT, Cummings SR.
(21) http://www.ncbi.nlm.nih.gov/pubmed/9609575 Am J Obstet Gynecol. 1998
May;178(5):1002-9.When does estrogen replacement therapy improve sleep quality?
Polo-Kantola P et al.
(22) http://cme.medscape.com/viewarticle/512093 "Menopausal Arthritis"
May Develop in Women Receiving Estrogen-Depleting Treatments News Author:
Laurie Barclay, MD CME Author: Désirée Lie, MD, MSEd
(23) http://www.emaxhealth.com/70/3606.html Women treated with aromatase
inhibitors often experience joint pain and musculoskeletal aching: severe
enough, in some cases, to make them stop the treatment.
(24) http://www.ncbi.nlm.nih.gov/pubmed/11173183 Maturitas. 2001 Jan
31;37(3):209-12. Treatment of keratoconjunctivitis sicca with topical androgen.
by Worda C et al.
(25) http://abstracts.iovs.org/cgi/content/abstract/44/5/2450 Invest Ophthalmol Vis Sci
2003;44: E-Abstract 2450. Treatment of Dry Eye with a Transdermal 3%
Testosterone Cream by C.G. Connor.
(26) http://eurheartj.oxfordjournals.org/content/31/12/1494.abstract Eur Heart J (2010) 31
(12): 1494-1501. Low serum testosterone levels are associated with increased
risk of mortality in a population-based cohort of men aged 20–79, Robin Haring
et al.
(27) http://circ.ahajournals.org/cgi/content/abstract/116/23/2694 Endogenous Testosterone
and Mortality Due to All Causes, Cardiovascular Disease, and Cancer in Men
European Prospective Investigation Into Cancer in Norfolk (EPIC-Norfolk)
Prospective Population Study (Circulation. 2007;116:2694-2701.)
(28) http://archinte.ama-assn.org/cgi/content/abstract/166/15/1660 Vol. 166 No. 15, Aug
14/28, 2006 Low Serum Testosterone and Mortality in Male Veterans Molly M.
Shores, MD et al. Arch Intern Med. 2006;166:1660-1665.
(29) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2755630 Menopause. 2009 Jan–Feb;
16(1): 15–23. Increased cardiovascular mortality following early bilateral
oophorectomy. Cathleen M. Rivera, MD et al.
(30) http://www.ncbi.nlm.nih.gov/pubmed/19384117 Obstet Gynecol. 2009
May;113(5):1027-37.Ovarian conservation at the time of hysterectomy and
long-term health outcomes in the nurses' health study. Parker WH et al.
(31) http://jama.ama-assn.org/content/303/1/47 Antidepressant Drug
Effects and Depression Severity A Patient-Level Meta-analysis. Jay C. Fournier
et al. JAMA. 2010;303(1):47-53.
(32) http://jama.ama-assn.org/content/305/3/267 Efficacy of Escitalopram
for Hot Flashes in Healthy Menopausal Women A Randomized Controlled Trial Ellen
W. Freeman, PhD; JAMA. 2011;305(3):267-274
(33) http://www.ncbi.nlm.nih.gov/pubmed/15551359 Int J Cancer. 2005 Apr
10;114(3):448-54. Breast cancer risk in relation to different types of hormone
replacement therapy in the E3N-EPIC cohort. Fournier A et al.
(34) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2211383/ Breast Cancer Res Treat.
2008 January; 107(1): 103–111. Unequal risks for breast cancer associated with
different hormone replacement therapies: results from the E3N cohort study.
Agnès Fournier et al.
(35) http://www.ncbi.nlm.nih.gov/pubmed/19752341 J Clin Oncol. 2009 Nov
1;27(31):5138-43. Estrogen-progestagen menopausal hormone therapy and
breast cancer: does delay from menopause onset to treatment initiation
influence risks? Fournier A et al.
(36) http://www.ncbi.nlm.nih.gov/pubmed/17651686 Ann Endocrinol (Paris).
2007 Sep;68(4):241-50. Epub 2007 Jul 24. Hormonal replacement therapy (HRT) in
postmenopause: a reappraisal. Caufriez A.
(37) http://jeffreydach.com/files/80618-70584/Hormones__in_wellness_and_disease_prevention_common_practices_current_state_evidence_Erika_Schwartz_Kent_Holtorf.pdf
Prim Care. 2008 Dec;35(4):669-705. Hormones in wellness and disease prevention:
common practices, current state of the evidence, and questions for the future.
Schwartz ET, Holtorf K.
(38) http://www.jpands.org/vol13no2/hotze.pdf Point/Counterpoint:The
Case for Bioidentical Hormones by Steven F. Hotze, M.D. Donald P. Ellsworth,
M.D. Journal of American Physicians and Surgeons Volume 13 Number 2 Summer 2008
p43.
(39) http://www.ncbi.nlm.nih.gov/pubmed/18775609 Could transdermal
estradiol + progesterone be a safer postmenopausal HRT? A review.
L'hermite M, Simoncini T, Fuller S, Genazzani AR. Maturitas. 2008
Jul-Aug;60(3-4):185-201.
(40) http://www.thorne.com/altmedrev/.fulltext/11/3/208.pdf A Comprehensive Review of
the Safety and Efficacy of Bioidentical Hormones for the Management of
Menopause and Related Health Risks Deborah Moskowitz, ND Altern Med Rev 2006;11(3):208-223
(41) http://online.wsj.com/article/SB123717056802137143.html March 16, 2009 The Truth
About Hormone Therapy Wall Street Journal By Erika Schwartz , Kent Holtorf ,
and David Brownstein
(42) http://www.tasciences.com/pdf/Harley_CMM_final.pdf Current Molecular
Medicine 2005, 5, 29-38 205 Telomerase Therapeutics for Degenerative Diseases.
By Calvin B. Harley.
(43) http://mcb.asm.org/cgi/content/full/20/11/3764 Molecular and Cellular
Biology, June 2000, p. 3764-3771, Vol. 20, No. 11 Induction of hTERT Expression
and Telomerase Activity by Estrogens in Human Ovary Epithelium Cells. Silvia
Misiti, et al.,
(44) http://cancerres.aacrjournals.org/content/59/23/5917.full Estrogen Activates
Telomerase. Satoru Kyo et al. Cancer Res December 1, 1999 59; 5917
(45) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC120798/ Microbiol Mol Biol Rev.
2002 September; 66(3): 407–425. Human Telomerase and Its Regulation. Yu-Sheng
Cong et al.
(46) http://www.nature.com/nature/journal/vaop/ncurrent/full/nature09603.html Telomerase reactivation
reverses tissue degeneration in aged telomerase-deficient mice by Ronald A.
DePinho et al. Nature November 2010.
AUthor: Jeffrey Dach MD

