Endometriosis is a chronic and incurable gynecological condition causing pelvic pain, menstrual irregularities, infertility and misery affecting 6-10% of women in the United States.(1)(7) The worldwide incidence of endometriosis is estimated to be between 0.1 and 0.3%, or about 150 to 200 million women.(17)
Medical treatments are largely ineffective. Surgical treatment with laparoscopy is used as a last resort to restore fertility and relieve pain.(2) In this article we will discuss natural treatments for endometriosis.
Above header image courtesy of Dr Seckin, Laparoscopic surgery for endometriosis.
What is Endometriosis ?
In this condition, the cells from the lining of the uterus called the endometrium are found at distant locations outside the uterus, with tissue deposits scattered throughout the peritoneal cavity. The mechanism, confirmed in animal experiments, is thought to be retrograde passage of menstrual endometrium through the fallopian tubes. These cells then seed the surface of the ovaries as well as the entire peritoneal cavity.(3)
“The primary theory of the pathogenesis of endometriosis…(is) the retrograde “regurgitation” of endometrial cells passing through the oviducts into the peritoneal cavity and proliferates in ectopic sites”. Quote from Dr. Ceccaroni (4)
Coexisting abnormalities of host immunity are also found. required to allow for abnormal implantation of the endometrial tissue. (1)
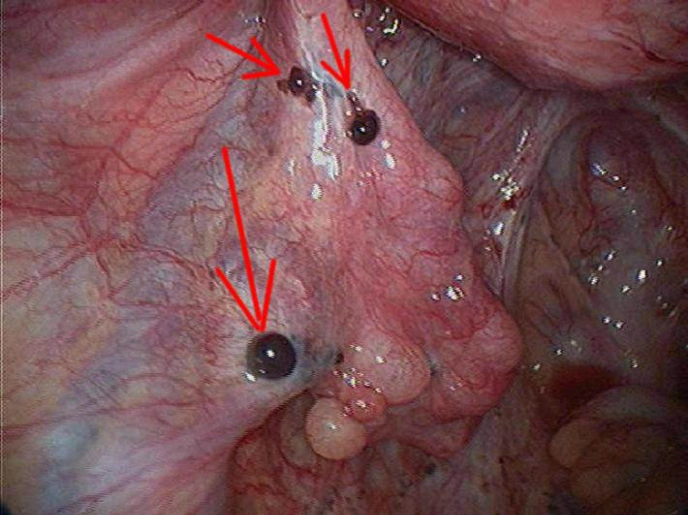
When doctors visualize the ovaries or the peritoneal lining with the laparoscope instrument, they may find implanted small dark nodules of endometrial tissue (see image below) . Microscopic examination of the endometrial implants shows induction of blood and nerve supply to the implants,
Left image: Shows Laparoscopic view of endometrial implants on peritoneal cavity ( Dark spots denoted by red arrows) courtesy of Dr. Yahya Kamal
Features Shared with Cancer
Although endometriosis is benign disease, it shares many of the features of cancer cells, and can be viewed as a neoplastic process.(5) There is extensive clinical, pathologic, and molecular evidence suggesting that endometriosis is a neoplastic process with a potential for malignant transformation.(5) Endometriosis may show up on cancer imaging with PET scanning giving a false positive scan.(6)
Resveratrol and ECGC, Fish Oil and Melatonin
If this is true, that endometriosis is a neoplastic process, then one might expect endometriosis to regress in response to natural substances that have anti-cancer activity, such as Resveratrol, ECGC (green tea), Fish oil and Melatonin. These have been studied in animal models.
Resveratrol is a natural substance obtained from red wine which has anti-proliferative and anti-inflammatory properties.(11) ECGC is an extract from green tea. A 2013 study by Dr Riccifound both Resveratrol and ECGC had a potent inhibitory effect on the development of endomeriosis in a mouse model. (7)
A 2011 study by Dr. Brune-Tran showed that Resveratrol inhibits development of experimental endometriosis in vivo and reduces endometrial stromal cell invasiveness in vitro. (8) In this study, nude mice were implanted with human endometriosis cells.(8) The authors found that Resveratrol decreased the number of endometrial implants by 60% and decreased total volume of implants by 80%.(8) This is quite an impressive result for a natural occurring supplement.
Fish Oil
Omega -3 Fatty acids in fish oil are known to have anti-inflammatory properties. A 2014 study by Dr. Jennifer L. Herington using an experimental mouse model of endometriosis, showed that in mice with a 10% supplemented fish oil diet, adhesion score and disease burden were significantly reduced. (9) The authors concluded,”an antiinflammatory diet that includes fish oil supplementation may be a beneficial adjuvant to reduce development of adhesions in women undergoing surgical treatment of endometriosis.”(9)
Melatonin
Melatonin has anti-cancer and anti-inflammatory properties and was studied by Dr. Guney in 2008 in a mouse model of endometriosis. (10) The authors found that Melatonin causes regression and atrophy of the endometriotic lesions in experimental mice.(10)
Adenomyosis
Adenomyosis is similar to endometriosis with similar ectopic implantation of endometrial tissue, in this case, the ectopic tissue resides within the uterus itself, in the muscular layer of the uterine wall where endometrial glandular tissue should not be found. Induction of adenomyosis in mice results in progressive hyperalgesia (increased sensitivity to pain), uterine hyperactivity, and elevated plasma corticosterone levels (indicating stress).(13-14)
ECGC, an extract of green tea has been found to possess anti-cancer activity (12). Two publications deal with ECGC as a beneficial natural treatment for adenomyosis.(13-14) In a 2013 study, Dr Chen found that EGCG suppresses myometrial infiltration, improves generalized hyperalgesia, reduced uterine contractility, and lowered plasma corticosterone levels in experimental mice induced with adenomyosis. (13-14)
Cyclic Natural Progesterone for Endometriosis
Another natural treatment which we have used successfully over the
years is cyclic progesterone, 20-40 mg twice a day applied as a topical
cream for days 8-26 of the menstrual cycle. This was pioneered by John R
Lee MD and described in his book, Natural Progesterone: The Multiple Roles of a Remarkable Hormone
Patients have reported good results with this regimen with relief of pain and other symptoms of endometriosis.
Dr Jeri Lynn Prior protocol with oral Prometium 300 mg BID.
Dr. Lam protocol for endometriosis – 20 mg topical progesterone BID days 8-26..
Women in Balance on Progesterone cream for endometriosis.
Medicinal Cannabis Beneficial for Endometriosis
If it is true that endometriosis is a benign disease that responds to natural substances with anti-cancer activity, then one would expect cannabis sativa extract to have beneficial effects. This is exactly what was found in multiple studies.(15-19) An additional benefit, reduction in pain was also reported. (15-19)
Pain from Endometriosis and the EndoCannabinoid System
Dr Dmitrieva studied the Endocannabinoid involvement in endometriosis and reported his findings in the journal Pain in 2010. He noted that previous endometriosis studies in mouse models and in women showed : “sensory and sympathetic nerve fibers sprout branches to innervate” the endometriosis implants.” In the past, medicinal cannabis was commonly used for control of endometriosis-associated pain. Dr. Dmitrieva theorized that the endocannabinoid system is involved in both endometriosis and its associated pain. Using a mouse model of endometriosis, Dr Dmitrieva found that CB1 cannabinoid receptors are expressed on the sensory and sympathetic nerves to the endometriosis implants.(15)
Progesterone and the Endometrium
Dioxin Disrupts Cannabinoid Signalling in the ENdometrium
In the Oct 2012 Fertility and Sterility, Dr. Kevin G. Osteen, proposed that exposure to environmental endocrine disruptor chemicals, such as dioxin, may trigger changes that promote progesterone-resistant endometriosis. He did a molecular study of the CB1 receptor Messenger RNA in endometriosis. He analysed Cannabinoid Receptor Messenger RNA (CB1-R mRNA) in human endometrial tissues before and after exposure to Dioxin, (TCDD) or a progesterone receptor antagonist drug, Onapristone.(16)
Dr. Osteen found that progesterone exposure in vivo during the secretory phase (days 12-26 of cycle) was associated with upregulation of endocannabinoid receptors in normal women. Dr. Osteen found increased genetic expression of endocannabinoid receptor (CB1-R) messenger RNA in endometrial tissue samples harvested from healthy normal women during days 12-26 of the menstrual cycle. However, there was no upregulation of gene expression in women with endometriosis. They found very little, or reduced expression of CB1-R gene expression in similar endometrial tissue samples taken from women with endometriosis.
The in vitro studies revealed that acute Dioxin exposure to normal endometrial cells produced this same abnormality, resulting in a failure of progesterone to up-regulate endocannabinoid receptor expression. The same results were obtained with a Progesterone antagonist drug.
The authors concluded that loss of normal progesterone responsiveness, ie. progesterone resistance, is a striking feature of endometriosis. In addition, the progesterone-mediated endometrial endocannabinoid receptor system was profoundly dysfunctional in women with endometriosis. Exposure to the endocrine disrupting chemical, Dioxin, replicated these abnormalities (16)
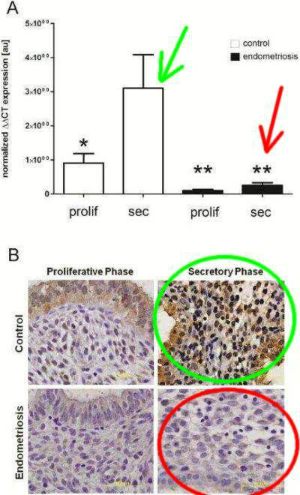 Left
Image: Upper Frame: Green arrow denotes normal increase in
endocannabinoid receptor gene expression in normal patients. Red arrow
denotes endometriosis patients with low gene expression during early
phase and no increase in secretory phase. Lower frame: Histology slide
of endometrial samples showing normal brown staining of receptor
proteins (green ellipse). And absent staining in tissues from
endometriosis patient (red ellipse Images courtesy of authors . and the NIH.(16) Link to Image.
Left
Image: Upper Frame: Green arrow denotes normal increase in
endocannabinoid receptor gene expression in normal patients. Red arrow
denotes endometriosis patients with low gene expression during early
phase and no increase in secretory phase. Lower frame: Histology slide
of endometrial samples showing normal brown staining of receptor
proteins (green ellipse). And absent staining in tissues from
endometriosis patient (red ellipse Images courtesy of authors . and the NIH.(16) Link to Image.
In 2012 in the journal Molecular Human Reproduction, Dr Sanchez from Milan Italy, published his review of the medical literature (metanalysis) on the molecular connections between the cannabinoid system and endometriosis.(17) Dr Sanchez says that endocannabinoid system and receptors (CB1 and CB2 receptors, etc). play a regulatory role for the endometrium throughout the menstrual cycle are these same receptors are present in the endometriosis tissue implants ouside the uterus in the peritoneal cavity. These endocannabinoid receptors are also present in sensory and sympathetic nerves supplying the endometrial emplants.(17) Various medicinal cannabinoids are found to be beneficial for endometriosis, producing both a reduction of cellular proliferation, and control of pain symptoms. Conversely, endometrial cell migration tends to be stimulated by drugs that block endocannabinoid receptors in the endometrium. (17)
β-Caryophyllene – Potent CB2 Receptor Agonist
Caryophyllene is a natural comnonent of cannabis oil as well as Copaiba Oil, which contains a cyclobutane ring which is quite rare in nature. Beta-caryophyllene is bioavailable, non-toxic and serves as a potent activator of CB2 endocannabinoid receptor system. These are receptors are present in the peripheral tissues and the immune system.
Published in 2013 European Journal of Pharmacology, Dr. Abbas reported his study using β-Caryophyllene in a mouse model of endometriosis.(18) Dr Abbas found β-Caryophyllene, a natural plant oil causes regression of endometrial implants with preservation of fertility.
He found that: ” β-Caryophyllene suppressed growth of endometriotic implants by 52.5% compared with controls. Also β-caryophyllene produced apoptosis in luminal epithelim of the cyst as well as in endothelial cells of blood vessels.”
He concluded: ” Therapy with β-caryophyllene may present a promising novel, non-toxic therapeutic option for patients with endometriosis.”(18)
This article is part one of a series.
For Part Two Click Here.
For Part Three Click here.
Articles With Related Interest:
Cannabis Research Suppressed
Cannabis Miracle Drug of the 21st Century
Jeffrey Dach MD
74590 Griffin Road Suite 190
Davie, Florida 33314
954-792-4663
References:
1) http://www.tandfonline.com/
Health, Risk & Society Volume 11, Issue 4, 2009 pages 367-385
Nobody really knows what it is or how to treat it’: Why women with endometriosis do not comply with healthcare advice Kate Seeara*
This paper examines the phenomenon of non-compliance with health advice
among 20 women who have been diagnosed with a chronic and incurable gynaecological condition called endometriosis.
Women’s non-compliance emerges out of their subjective experiences of
self-care and risk-avoidance injunctions as burdensome and excessive, as
well as practically impossible, time-consuming and too expensive.
Non-compliance is also motivated by a desire to avoid exposure to
potential risks that can arise from compliance itself. Women also resist
risk-avoidance advice on the basis of their scepticism and mistrust of
doctors, whose expertise about endometriosis they doubt. This analysis
contributes to our understanding of patient non-compliance and has
ramifications for how health promotion and risk-avoidance campaigns are
constructed and implemented, especially where chronic illnesses are
concerned.
2) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3135985/
Indian J Med Res. Jun 2011; 133(6): 581–593.
Endometriosis, a modern syndrome. by Ivo Brosens and Giuseppe Benagiano
Leuven Institute for Fertility & Embryology, Leuven, Belgium
Department of Gynaecology, Obstetrics & Urology, ‘Sapienza’
University of Rome, Italy
3) http://www.ncbi.nlm.nih.gov/pubmed/24389257
Front Biosci (Schol Ed). 2014 Jan 1;6:16-28.
Menstrual endometrial supernatant may induce stromal endometriosis in
baboons. Kyama CM1, Falconer H2, Cuneo S2, Chai D2, Mihalyi A1, Mwenda
J2, D’Hooghe T3.
We tested the hypothesis that endometriosis can be induced in baboons more successfully by intra-pelvic injection of the pellet of menstrual endometrium when compared to its supernatant. Menstrual endometrium, separated into pellet (n = 5) and supernatant fractions ( n = 8), or phosphate buffered saline (1 ml, n = 7, controls) was injected laparoscopically into the pelvis. During laparoscopy 25 days later, the number (ρ = 0.027) and surface area (ρ <0.0001) of endometriosis-like lesions were significantly higher in the pellet group, than in the supernatant group, or in the control group. Histological typical endometriosis was present only in the endometrial pellet group (1/15), whereas stromal endometriosis was observed in both the pellet group (6/15), and the supernatant group (6/20). Peritoneal endometrial like glands were observed in both the endometrial pellet group (3/15), and in the supernatant group (1/20). In conclusion, we confirmed our hypothesis that endometriosis can be induced in baboons more successfully by intrapelvic injection of the pellet of menstrual endometrium when compared to its supernatant.
4) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3516977/
Wideochir Inne Tech Malo Inwazyjne. Jun 2012; 7(2): 122–131.
Pericardial, pleural and diaphragmatic endometriosis in association with
pelvic peritoneal and bowel endometriosis: a case report and review of
the literature. Marcello Ceccaroni,corresponding author1,2 Giovanni
Roviglione,1,2 Piergiorgio Rosenberg,3 Anna Pesci,4 Roberto Clarizia,1,5
Francesco Bruni,1,2 Claudio Zardini,6 Giacomo Ruffo,6 Angelo Placci,7
Stefano Crippa,6 and Luca Minelli2
5) http://www.reproduction-
Reproduction March 1, 2004 127 293-304
Endometriosis and the neoplastic process by Rajesh
Varma1,2, Terrance Rollason3, Janesh K Gupta2 and Eamonn R Maher.
Section of Medical and Molecular Genetics, 2Academic Department of
Obstetrics and Gynaecology and 3Department of Histopathology,
Birmingham Women’s Hospital, Birmingham B15 2TG, UK.
Although endometriosis is a benign disorder, recent studies of endometriosis suggest endometriosis could be viewed as a neoplastic process.
In summary, there is extensive clinicopathological, molecular and genetic evidence supporting the hypothesis that endometriosis is a neoplastic process with a potential for malignant transformation.
endometriosis False positive PET scan
6) http://www.ncbi.nlm.nih.gov/
Eur J Obstet Gynecol Reprod Biol. 2004 Dec 1;117(2):236-9.
Endometriosis with FDG uptake on PET.
Jeffry L1, Kerrou K, Camatte S, Metzger U, Lelièvre L, Talbot JN, Lecuru
F. The value of [18F]fluorodeoxyglucose positron emission tomography
(FDG-PET) uptake in endometriosis has not yet been extensively reported.
CASE REPORT:A 32-year-old woman was examined to find an explanation for
right pelvic pain associated with right subcostal pain. A computerised
tomography (CT) scan was compatible with a haemangioma or a focus of
endometriosis in the liver. Transvaginal sonography and magnetic
resonance imaging (MRI) showed a complex ovarian cyst on the left. Blood
CA125 levels were elevated. FDG-PET revealed a focus of uptake in the
right paravesical area. Laparoscopy showed a left endometrioma
associated with diffuse inflammatory pelvic adhesions. After surgery and
3 months GnRH agonist treatment the pain had disappeared and neither
MRI nor FDG-PET showed any pelvic abnormality. The patient subsequently
presented with dyspareunia and rectal pain resulting from a right uterosacral nodule and a rectal nodule. These were resected laparoscopically. After a 1-year follow-up, the patient is doing well.
CONCLUSION: Endometriosis can give rise to false-positive results on FDG-PET.
However, the FDG uptake in this particular case of endometriosis seems
to have been due to inflammation rather than to a cyst. This report
highlights the relationship between some of the biological features of
endometriosis and some observed in neoplastic lesions.
Resveratrol – ECGC (maybe Pterstilnbene)
7) http://humrep.oxfordjournals.
Hum Reprod. 2013 Jan;28(1):178-88. doi: 10.1093/humrep/des369. Epub 2012
Oct 18. Natural therapies assessment for the treatment of
endometriosis. Ricci AG1, Olivares CN, Bilotas MA, Bastón JI, Singla
JJ, Meresman GF, Barañao RI.
Can resveratrol and epigallocatechin-3-gallate (EGCG) inhibit the
growth and survival of endometriotic-like lesions in vivo in a BALB/c
model of endometriosis, and in vitro in primary cultures of human
endometrial epithelial cells (EECs)?
SUMMARY ANSWER:Resveratrol and EGCG exerted a potent inhibitory effect
on the development of endometriosis in a BALB/c murine model and on the
survival of EECs.
WHAT IS KNOWN ALREADY:Endometriosis is a common condition associated
with infertility and pelvic pain in women of reproductive age.
Resveratrol and EGCG are two polyphenols with anticarcinogenic and
antioxidant properties that have been proposed as natural therapies to
treat endometriosis.
STUDY DESIGN, SIZE, DURATION: Fifty-six 2-month-old female BALB/c mice
underwent surgical induction of endometriosis. Treatments with
resveratrol or EGCG started 15 days post-surgery and continued for 4
weeks. Human biopsies were taken with a metal Novak curette from the
posterior uterine wall from 16 patients with untreated endometriosis and
15 controls who underwent diagnostic laparoscopy for infertility.
MATERIALS, SETTING, METHODS: After the treatments, animals were
sacrificed and lesions were counted, measured, excised and fixed.
Immunohistochemistry for proliferating cell nuclear antigen and CD34 was
performed for cell proliferation and vascularization assessment in the
lesions. The terminal deoxynucleotidyl transferase (TdT)-mediated dUTP
nick-end labeling (TUNEL) technique was performed for apoptosis
evaluation. Peritoneal fluid was collected to analyze vascular
endothelial growth factor levels. Human EECs were purified from
proliferative-phase endometrial biopsies and cultured. The effect of
both polyphenols on cell proliferation was determined by a colorimetric
assay using the CellTiter 96®AQueous One Solution Cell Proliferation
Assay kit and on apoptosis by the TUNEL technique, using an In Situ Cell
Death Detection Kit with Fluorescein.
MAIN RESULTS: In the mouse model, both treatments significantly reduced
the mean number (P < 0.05 versus control) and the volume of
established lesions (P < 0.05 versus control). Treatments
consistently statistically significantly diminished cell proliferation
(resveratrol P < 0.01 and EGCG P < 0.05, versus control), reduced
vascular density (resveratrol P < 0.01 and EGCG P < 0.001, versus
control) and increased apoptosis within the lesions (resveratrol P <
0.01 and EGCG P < 0.05, versus control). Both compounds induced
reduction in human EEC proliferation (P < 0.05 versus basal) and
increased apoptosis (P < 0.05 versus basal) in primary cultures.
LIMITATIONS: In vitro studies were only carried out in epithelial cells from human eutopic endometrium.
WIDER IMPLICATIONS OF THE FINDINGS: The present findings are promising
and will assist the development of novel natural treatments for
endometriosis.
STUDY FUNDING: This study was supported by ANPCYT (PICT 6384 BID 1201
OC-AR) and CONICET (PIP 5471), Argentina. None of the authors has any
conflict of interest to declare.
Endometriosis is one of the most common benign disorders and affects 6–10% of women of reproductive age (Giudice and Kao, 2004). The disease is defined as the presence of endometrial glands and stroma outside the uterine cavity and patients with endometriosis often suffer from dysmenorrhea, dyspareunia, dysuria and chronic abdominal or pelvic pain, as well as infertility, resulting in a limited quality of life (Giudice and Kao, 2004). As the disease is estrogen-dependent, medical therapies are principally aimed at down-regulating ovarian estrogen production (Valle and Sciarra, 2003; Mihalyi et al., 2006).
EGCG from green tea and resveratrol from red wine and grapes are some of the natural options that have lately been considered to treat different types of cancer
We observed that both resveratrol and EGCG exerted a significant inhibition on the development of endometriotic-like lesions, reducing the size of the lesions, by diminishing cell proliferation and increasing apoptotic levels. Moreover, both treatments were able to decrease the number of established lesions per mouse. It is remarkable that a treatment that begins 15 days after surgery can affect the development and maintenance of already established endometriotic-like lesions rather than just their establishment.
8) http://www.ncbi.nlm.nih.gov/
Biol Reprod. 2011 Jan;84(1):106-12. Epub 2010 Sep 15.
Resveratrol inhibits development of experimental endometriosis in vivo and reduces endometrial stromal cell invasiveness in vitro.
Bruner-Tran KL1, Osteen KG, Taylor HS, Sokalska A, Haines K, Duleba AJ.
Endometriosis is a common gynecologic disorder characterized by ectopic attachment and growth of endometrial tissues. Resveratrol is a natural polyphenol with antiproliferative and anti-inflammatory properties. Our objective was to study the effects of resveratrol on human endometriotic implants in a nude mouse model and to examine its impact on human endometrial stromal (HES) cell invasiveness in vitro. Human endometrial tissues were obtained from healthy donors. Endometriosis was established in oophorectomized nude mice by intraperitoneal injection of endometrial tissues. Mice were treated with 17β-estradiol (8 mg, silastic capsule implants) alone (n = 16) or with resveratrol (6 mg/mouse; n = 20) for 10-12 and 18-20 days beginning 1 day after tissue injection. Mice were killed and endometrial implants were evaluated. A Matrigel invasion assay was used to examine the effects of resveratrol on HES cells. We assessed number and size of endometriotic implants in vivo and Matrigel invasion in vitro. Resveratrol decreased the number of endometrial implants per mouse by 60% (P < 0.001) and the total volume of lesions per mouse by 80% (P < 0.001). Resveratrol (10-30 μM) also induced a concentration-dependent reduction of invasiveness of HES by up to 78% (P < 0.0001). Resveratrol inhibits development of endometriosis in the nude mouse and reduces invasiveness of HES cells. These observations may aid in the development of novel treatments of endometriosis.
fish oil
9) http://www.ncbi.nlm.nih.gov/
Fertil Steril. PMC Feb 1, 2014. Fertil Steril. Feb 2013; 99(2):
543–550.e1. Dietary fish oil supplementation inhibits formation of
endometriosis-associated adhesions in a chimeric mouse model. Jennifer
L. Herington, Ph.D.,a Dana R. Glore, B.S.,a John A. Lucas, M.D.,a Kevin
G. Osteen, Ph.D.,a,b and Kaylon L. Bruner-Tran, Ph.D.a
Melatonin
10) http://www.ncbi.nlm.nih.gov/
Fertil Steril. 2008 Apr;89(4):934-42. Epub 2007 Jun 19.
Regression of endometrial explants in a rat model of endometriosis
treated with melatonin. Güney M1, Oral B, Karahan N, Mungan T.
To determine the antioxidant, antiinflammatory, and immunomodulatory
effects of melatonin on endometrial explants, the distribution of
cyclooxygenase-2 (COX-2), the activity of antioxidant enzymes superoxide
dismutase (SOD) and catalase (CAT), and levels of malondialdehyde (MDA)
in the rat endometriosis model.
DESIGN:Prospective, placebo-controlled experimental study.
SETTING:Experimental surgery laboratory in a university department.
ANIMAL(S):Twenty-five rats with experimentally induced endometriosis.
INTERVENTION(S):Endometriosis was surgically induced in 25 rats
by transplanting an autologous fragment of endometrial tissue onto the
inner surface of the abdominal wall. Four weeks later, three
rats were killed and the remaining 22 rats given second-look
laparotomies to identify and measure ectopic uterine tissue in three
dimensions. After the second laparotomy, 4 weeks of vehicle and
melatonin treatment were administered, then all of the rats were given a
third laparotomy and killed.
MAIN OUTCOME MEASURE(S):The volume and weight of the implants were
measured. The remaining rats were randomly divided into two groups. In
control group (group 1; n = 11) no medication was given. To the rats in
melatonin-treated group (group 2; n = 11), 10 mg/kg a day of melatonin
was administered intraperitoneally. Four weeks later, after the second
laparotomy, the endometrial explants were reevaluated morphologically,
and COX-2 expression was evaluated immunohistochemically and
histologically. In addition, endometrial explants were analyzed for the
antioxidant enzymes SOD, CAT, and MDA, a marker of lipid peroxidation. A
scoring system was used to evaluate expression of COX-2 and
preservation of epithelia.
RESULT(S):The pretreatment and posttreatment volumes within the control
group were 135.9 +/- 31.5 and 129.4 +/- 28.7, respectively. The mean
explant volume was 141.4 +/- 34.4 within the melatonin group before the
treatment and 42.9 +/- 14.0 after 4 weeks of treatment. There was a
statistically significant difference in spherical volumes (129.4
+/- 28.7 versus 42.9 +/- 14.0 mm(3)) of explant weights (155.8 +/- 27.1
versus 49.6 +/- 19.5 mg) and COX-2 positivity (91% versus 18.1%)
between groups after the third laparotomy. In the melatonin-treated
group, the endometrial explant levels of MDA statistically significantly
decreased and activities of SOD and CAT significantly increased when
compared with the control group. The epithelia showed statistically
significantly better preservation in the control group when compared
with the melatonin-treated group (2.54 +/- 0.52 versus 0.63 +/- 0.50). CONCLUSION(S):Melatonin causes regression and atrophy of the endometriotic lesions in rats.
Molecular Mechanisms of reveratrol
11) http://www.ncbi.nlm.nih.gov/pubmed/20443159
Crit Rev Food Sci Nutr. 2009 Oct;49(9):782-99. Fighting cancer with red wine? Molecular mechanisms of resveratrol.
Kraft TE1, Parisotto D, Schempp C, Efferth T.
Resveratrol, a red wine constituent, has been known for its
cardioprotective effects. Recent data give ample evidence that
resveratrol can act as a chemopreventive agent as well. Tumor initation,
promotion, and progression are affected by resveratrol via multiple
pathways, which are discussed in this review. Resveratrol has anti-inflammatory
effects by counteracting NF-kappa B and AP-1 transcription and can
prevent bioactivation of procarcinogens by interacting with drug
metabolizing enzymes. Furthermore, resveratrol exerts antioxidant
activities, hence contributing to the prevention of tumor initiation. Growing
or metastasizing carcinomas are inhibited by resveratrol through
prevention of angiogenesis by inhibiting VEGF and matrix
metalloproteases. Induction of apoptosis and cell cycle arrest,
important mechanisms for cancer therapy, are stimulated by
resveratrol through different mechanisms, e.g., activation of p53 and
modulation of cell cycle proteins. Although there has been remarkable
evidence for resveratrol as a potent chemopreventive agent in vitro, it
seems that the low bioavailability of resveratrol in humans could
interfere with a successful in vivo treatment. Nevertheless, resveratrol
offers two major advantages over conventional chemotherapy. The
cytotoxic effects of resveratrol on healthy cells can be neglected, and,
as several pathways leading to chemotherapeutic effects are activated
by resveratrol, chemoresistance-inducing mutations in cancer cells can
be overcome.
Adenomyosis ECGC
12) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3304302/
Adv Clin Chem. 2011;53:155-77.
EGCG, green tea polyphenols and their synthetic analogs and prodrugs for human cancer prevention and treatment.
Chen D1, Wan SB, Yang H, Yuan J, Chan TH, Dou QP.
Cancer-preventive effects of tea polyphenols, especially
epigallocatechin-3-gallate (EGCG), have been demonstrated by
epidemiological, preclinical, and clinical studies. Green tea
polyphenols such as EGCG have the potential to affect multiple
biological pathways, including gene expression, growth factor-mediated
pathways, the mitogen-activated protein kinase-dependent pathway, and
the ubiquitin/proteasome degradation pathway. Therefore, identification
of the molecular targets of EGCG should greatly facilitate a better
understanding of the mechanisms underlying its anticancer and
cancer-preventive activities. Performing structure-activity relationship
(SAR) studies could also greatly enhance the discovery of novel tea
polyphenol analogs as potential anticancer and cancer-preventive agents.
In this chapter, we review the relevant literature as it relates to the
effects of natural and synthetic green tea polyphenols and EGCG analogs
on human cancer cells and their potential molecular targets as well as
their antitumor effects. We also discuss the implications of green tea
polyphenols in cancer prevention.
13) http://rsx.sagepub.com/
Possible Loss of GABAergic Inhibition in Mice With Induced Adenomyosis and Treatment With Epigallocatechin-3-Gallate Attenuates the Loss With Improved Hyperalgesia. Reproductive Sciences February 3, 2014 . Yumei
Chen, MD1 Bo Zhu, MD1 Hongping Zhang, MD1 Ding Ding, MD,
PhD2 Xishi Liu, MD, PhD2 Sun-Wei Guo, PhD2⇑ 1Department of
Obstetrics and Gynecology, The People’s Hospital, Wenzhou, Zhejiang,
China
2Shanghai OB/GYN Hospital, Fudan University, Shanghai, China
Sun-Wei Guo, Shanghai Obstetrics and Gynecology Hospital, Fudan University, 419 Fangxie Road, Shanghai 200011, China.
Abstract We have previously reported that induction of adenomyosis in mice results in progressive hyperalgesia, uterine hyperactivity, and elevated plasma corticosterone levels and that epigallocatechin-3-gallate (EGCG) treatment dose dependently suppressed myometrial infiltration and improved generalized hyperalgesia. In this study, we examined whether adenomyosis induced in mice results in the loss of GABAergic inhibition as manifested by the diminished glutamate decarboxylase (GAD) 65-expressing neurons in the brainstem nucleus raphe magnus (NRM) that could correlate with heightened hyperalgesia. We also evaluated whether EGCG treatment would reverse these changes and also improve the expression of some proteins known to be involved in adenomyosis. Adenomyosis was induced in 28 female ICR mice and additional 12 were used as blank controls, as reported previously. At the 16th week, all mice with induced adenomyosis received low- or high-dose EGCG treatment or untreated. Mice without adenomyosis received no treatment. After 3 weeks of treatment, their uterine horns and brains were harvested. The right uterine horn was used for immunohistochemistry analysis and for counting the number of macrophages infiltrating into the ectopic endometrium. The brainstem NRM sections were subjected to immunofluorescence staining for GAD65. We found that mice with induced adenomyosis had significantly diminished GAD65-expressing neurons, concomitant with heightened hyperalgesia. Treatment with EGCG increased these neurons in conjunction with improved hyperalgesia, reduced the expression of p-p65, cycloxygenase 2, oxytocin receptor, collagen I and IV, and transient receptor potential vanilloid type 1 in ectopic endometrium or myometrium, reduced the number of macrophages infiltrating into the ectopic endometrium while elevated the expression of progesterone receptor isoform B. Thus, adenomyosis-induced pain resembles neuropathic pain in that there is a remarkable central plasticity.
14) http://www.ncbi.nlm.nih.gov/
Reprod Sci. 2013 Dec;20(12):1478-91. Epub 2013 May 23.
Epigallocatechin-3-gallate reduces myometrial infiltration, uterine
hyperactivity, and stress levels and alleviates generalized hyperalgesia
in mice induced with adenomyosis.
Chen Y1, Zhu B, Zhang H, Liu X, Guo SW.
In an effort to search for novel therapeutics for adenomyosis, we sought
to determine whether treatment with epigallocatechin-3-gallate (EGCG)
would suppress the myometrial infiltration, improve pain behavior, lower
stress level, and reduce uterine contractility in a mice model of
adenomyosis. Adenomyosis was induced in 28 female ICR mice neonatally dosed with tamoxifen, while another 12 (group C) were dosed with solvent only, which served as a blank control. Starting from 4 weeks after birth, hot plate test was administrated to all mice every 4 weeks.
At the 16th week, all mice induced with adenomyosis were randomly
divided into 3 groups: low-dose EGCG (5 mg/kg), high-dose EGCG (50
mg/kg), and untreated. Group C received no treatment. After 3 weeks of
treatment, the hot plate test was administered again, a blood sample was
taken to measure the plasma corticosterone level by enzyme-linked
immunosorbent assay, and then all mice were sacrificed. The depth of
myometrial infiltration and uterine contractility were also evaluated.
We found that the induction of adenomyosis resulted in
progressive generalized hyperalgesia, along with elevated amplitude and
frequency of uterine contractions as well as elevated plasma
corticosterone levels. The EGCG treatment dose dependently
suppressed myometrial infiltration, improved generalized hyperalgesia,
reduced uterine contractility, and lowered plasma corticosterone levels.
These results suggest that induced adenomyosis causes pain and elevates
stress levels in mice. Uterine hyperactivity may contribute to
dysmenorrhea in women with adenomyosis who might also have elevated
stress level due to pain. The EGCG appears to be a promising compound
for treating adenomyosis.
————————–
Medical Cannabis for Endometriosis
Endocannabinoisd System in Endometriosis
15) http://www.ncbi.nlm.nih.gov/
http://www.ncbi.nlm.nih.gov/
Pain. 2010 Dec;151(3):703-10. doi: 10.1016/j.pain.2010.08.037. Epub 2010 Sep 15. Endocannabinoid involvement in endometriosis.
Dmitrieva N1, Nagabukuro H, Resuehr D, Zhang G, McAllister SL, McGinty KA, Mackie K, Berkley KJ.
Endometriosis is a disease common in women that is defined by abnormal
extrauteral growths of uterine endometrial tissue and associated with
severe pain. Partly because how the abnormal growths become associated
with pain is poorly understood, the pain is difficult to alleviate without resorting to hormones or surgery, which often produce intolerable side effects or fail to help. Recent
studies in a rat model and women showed that sensory and sympathetic
nerve fibers sprout branches to innervate the abnormal growths.
This situation, together with knowledge that the endocannabinoid system
is involved in uterine function and dysfunction and that exogenous
cannabinoids were once used to alleviate endometriosis-associated pain,
suggests that the endocannabinoid system is involved in both
endometriosis and its associated pain.
Herein, using a rat model, we found that CB1 cannabinoid receptors are expressed on both the somata and fibers of both the sensory and sympathetic neurons that innervate endometriosis’s abnormal growths. We further found that CB1 receptor agonists decrease, whereas CB1 receptor antagonists increase, endometriosis-associated hyperalgesia. Together these findings suggest that the endocannabinoid system contributes to mechanisms underlying both the peripheral innervation of the abnormal growths and the pain associated with endometriosis, thereby providing a novel approach for the development of badly-needed new treatments.
First, CB1 receptors were abundantly found not only on sensory and sympathetic fibers that had sprouted to innervate the ectopic growths (cysts), but also on retrogradely-identified somata of DRG and CG neurons from which the sprouted fibers originate. This finding indicates that CB1 receptors are strategically located for endogenous cannabinoids to influence functioning of cyst-innervating neurons. Second, CB1 labeling was significantly denser in the cysts than in the eutopic uterus. This finding indicates an upregulation of CB1 receptors in the ectopic uterine tissue relative to the healthy uterine tissue, which suggests that the endocannabinoid system is involved in the development and functioning of the abnormal sprouted innervation.
16) http://www.ncbi.nlm.nih.gov/
Fertil Steril. Oct 2012; 98(4): 948–956.e1.
Progesterone-dependent Regulation of Endometrial Cannabinoid Receptor
Type 1 (CB1-R) Expression is Disrupted in Women with Endometriosis and
in Isolated Stromal Cells Exposed to TCDD (2,3,7,8-tetrachlorodibenzo-p-
David Resuehr, PhD, Dana R. Glore, BS, Hugh S. Taylor, MD, PhD,† Kaylon L. Bruner-Tran, PhD, and Kevin G. Osteen, PhD
Women’s Reproductive Health Research Center, Department of Obstetrics
and Gynecology, Vanderbilt University School of Medicine, Nashville, TN
USA
†Department of Obstetrics, Gynecology and Reproductive Sciences, Yale University School of Medicine, New Haven CT, USA
To whom correspondence and reprint requests should be addressed: Kevin
G. Osteen, PhD Women’s Reproductive Health Research Center Department of
Obstetrics and Gynecology Vanderbilt University School of Medicine 1161
21st Ave S; MCN B-1100 Nashville, TN 37232
Conclusions:Our studies reveal a role for the anti-inflammatory
actions of progesterone in regulating endometrial cannabinoid signaling,
which is disrupted in women with endometriosis. Significantly, our
studies demonstrate, for the first time, that acute TCDD exposure
disrupts cannabinoid signaling in the human endometrium.
Endometriosis, characterized by the presence of endometrial glands and
stroma at extrauterine sites, is a common and debilitating reproductive
disease of uncertain etiology. Although typically considered an
endocrine disorder, women with endometriosis frequently exhibit immune
system dysfunctions that not only affect the initial development of the
disease but may contribute to the impaired fertility and severe pelvic
pain that are frequently noted as co-morbidities [1–2]. Although
estrogen has long been considered to represent the most important
steroid in the pathogenesis of endometriosis [2–3], research over the
past decade suggests that reduced progesterone sensitivity may play an
equally relevant role in the initiation and progression of this disease
[4–7].
Based on a review of evidence from multiple laboratories, we recently
proposed that exposure to dioxin-like environmental toxicants,
including 2,3,7,8-tetrachlorodibenzo-p-
17) http://molehr.oxfordjournals.
http://www.ncbi.nlm.nih.gov/
The molecular connections between the cannabinoid system and endometriosis A.M. Sanchez1,P. Vigano2,*, A. Mugione1, P. Panina-Bordignon1 and M. Candiani2 1Reproductive Sciences Laboratory, Obstetrics and Gynecology Unit, San Raffaele Scientific Institute, Milan, Italy
The endocannabinoid system consists of an array of endogenously
produced bioactive lipids that activate cannabinoid 1 (CB1) and 2 (CB2)
receptors. Alterations of this system have been described in almost
every category of disease. These changes can be protective or
maladaptive, making the endocannabinoid network an attractive
therapeutic target. Little is known about the potential role of
endocannabinoids in endometriosis development although this is a topic
worthy of further investigation since endocannabinoid modulators have
recently been shown to affect specific mechanisms critical to
endometriosis establishment and maintenance. A literature review was
herein performed with the aim of defining the regulation and function of
the endocannabinoid signaling in in vitro and animal models of
endometriosis. The components of the endocannabinoid system, CB1 and CB2
receptors and the enzymes N-
The endocannabinoid system and endometriosis-related pain
Endometriosis is usually associated with pelvic pain such as chronic dysmenorrhea, intermenstrual abdominal and pelvic pain, back pain, dysuria, dyschezia and dyspareunia.
The neural mechanisms of pain in endometriosis have been extensively described elsewhere (Stratton and Berkley, 2011). Three mechanisms, nociceptive, inflammatory and neuropathic, seem to be relevant to endometriosis-associated pelvic pain (Howard, 2009).
These findings suggest that cannabinoids could suppress endometriosis-induced hyperalgesia via the CB1 receptor (Dmitrieva et al., 2010). A promising new direction for developing new treatments for pain suffered by women with endometriosis may arise from these data.
β-Caryophyllene constituent of essential oil of Cannabis sativa,
18) http://www.ncbi.nlm.nih.gov/
Eur J Pharmacol. 2013 Feb 28;702(1-3):12-9. doi: 10.1016/j.ejphar.2013.01.011. Epub 2013 Jan 23.
β-Caryophyllene causes regression of endometrial implants in a rat model of endometriosis without affecting fertility.
Abbas MA1, Taha MO, Zihlif MA, Disi AM.
Many studies have shown that anti-inflammatory agents are effective in the treatment of endometriosis. β-Caryophyllene exerted a potent anti-inflammatory effect in vivo. However, its effect on endometriosis has not been investigated. This study aims at investigating the effect of β-caryophyllene on endometriosis and on fertility and reproduction in adult female rats.
Autologous fragments of the endometrium were implanted in the peritoneal cavity in adult female rats. The growth of the endometriotic implants that developed after four weeks was recorded. Treatment started then with β-caryophyllene (10 mg/kg or 30 mg/kg) or vehicle (control) for 21 days and the growth of the endometriotic implants was measured again. In fertility studies, female rats that received β-caryophyllene or vehicle were mated and reproductive functions were observed including number and viability of implants, number of corpora lutea, length of pregnancy and outcome of litter.
β-Caryophyllene (10 mg/kg) suppressed the growth of endometriotic implants by 52.5% compared with controls. Also β-caryophyllene produced apoptosis in luminal epithelim of the cyst as well as in endothelial cells of blood vessels. Ultrastructural studies revealed the presence of active mast cells and eosinophils in both control and β-caryophyllene-treated rat cysts. No statistically significant difference was observed in any studied parameter between control and β-caryophyllene-treated groups in fertility study. Therapy with β-caryophyllene may present a promising novel, non-toxic therapeutic option for patients with endometriosis.
link to this article:
http://wp.me/p3gFbV-1qu
Jeffrey Dach MD
http://www.jeffreydach.com/
http://www.drdach.com/
http://www.naturalmedicine101.com/
http://www.truemedmd.com/ http://www.bioidenticalhormones101.com
Disclaimer click here: http://www.drdach.com/wst_page20.html
The reader is advised to discuss the comments on these pages with
his/her personal physicians and to only act upon the advice of his/her
personal physician. Also note that concerning an answer which appears as
an electronically posted question, I am NOT creating a physician —
patient relationship.
Although identities will remain confidential as much as possible, as I can not control the media, I can not take responsibility for any breaches of confidentiality that may occur.
Link to this article:
http://wp.me/p3gFbV-1qu
Copyright (c) 2014 Jeffrey Dach MD All Rights Reserved
This article may be reproduced on the internet without permission,
provided there is a link to this page and proper credit is given.
FAIR USE NOTICE: This site contains copyrighted material the use of which has not always been specifically authorized by the copyright owner. We are making such material available in our efforts to advance understanding of issues of significance. We believe this constitutes a ‘fair use’ of any such copyrighted material as provided for in section 107 of the US Copyright Law. In accordance with Title 17 U.S.C. Section 107, the material on this site is distributed without profit to those who have expressed a prior interest in receiving the included information for research and educational purposes.